
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 2, March/April 2021
84
AFRICA
patients had cardiac injury and first demonstrated that cardiac
injury was independently associated with an increased risk of
mortality in patients with COVID-19.
10
Compared with patients without cardiac injury, those with
cardiac injury presented with more severe disease, manifested by
abnormal laboratory and radiographic findings, such as higher
levels of CRP, NT-proBNP and creatinine, more severe pneumonia,
and a greater proportion required mechanical ventilation.
Consistently, our study demonstrated that cardiac biomarkers
such as hs-TNT and NT-proBNP were associated with clinical
outcomes in COVID-19 and had correlations with other
inflammatory markers such as fibrinogen, D-dimer, ferritin,
procalcitonin and CRP. Higher mortality and ICU admission
rates were seen in patients with cardiac injury.
Severe respiratory distress is mostly considered the leading
cause of COVID-19-induced death. According to a published
study of the largest clinical trial in China,
11
severe pneumonia was
independently associated with admission to an ICU, mechanical
ventilation or death.
The laboratory results of patients who were classified in thorax
CT scans according to severity of infiltration were compared,
and as the severity of infiltration increased, an increase in level
of cardiac biomarkers and inflammatory markers was shown in
our study and in the literature.
This study shows that patients with co-morbid conditions
were more predisposed to experience myocardial injury during
the progression of COVID-19. For patients with underlying
chronic illness, including hypertension, coronary heart disease and
cardiomyopathy, the viral disease can further damage myocardial
cells through several mechanisms, including direct damage by the
virus, cytokine storm damage by systemic inflammatory responses,
destabilised coronary plaque leading to MI, and aggravated
hypoxia leading to myocardial ischaemia and infarction.
Although the accurate pathophysiological mechanism
underlying myocardial injury caused by COVID-19 is not fully
understood, a previous report showed that in 35% of patients
with severe acute respiratory syndrome coronavirus (SARS-
CoV) infection, the SARS-CoV genome was positively detected
in the heart. This raises the possibility of direct damage of the
cardiomyocytes by the virus.
12
SARS-CoV-2 may share the same
140.00
120.00
100.00
80.00
60.00
40.00
1.00 2.00 3.00
Thorax CT
Mean of C-reactive protein, mg/l
2.50
2.00
1.50
1.00
0.50
0.00
1.00 2.00 3.00
Thorax CT
Mean of prokcalcitonim, ng/ml
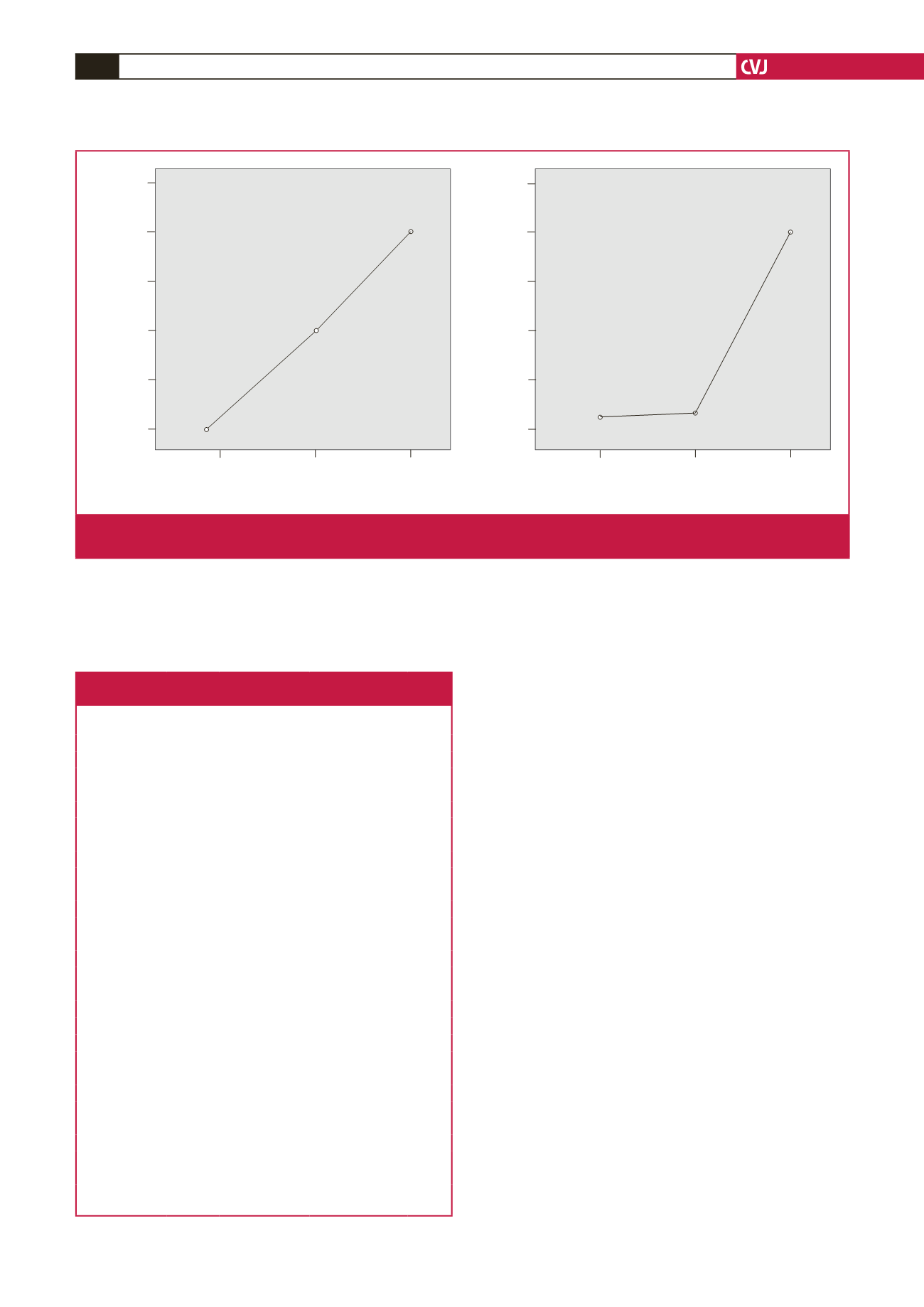
Thorax CT: 1 (mild pneumonia), 2 (moderate pneumonia), 3 (severe pneumonia)
Fig. 3.
Mean plots of serum levels of C-reactive protein and procalcitonin compared with patients grouped according to thorax CT
scans, which were divided into three categories: 1, mild pneumonia; 2, moderate pneumonia; and 3, severe pneumonia.
Table 5. Laboratory findings of patients grouped
according to thorax CT scans
Biomarker
Thorax
CT group Median (range)
Multiple compari-
son (Bonferroni) p-value
hsTNT, pg/ml
1
15 (3–228)
Thorax CT (1–2)
0.55
2
53 (3–3417)
Thorax CT (1–3)
0.42
3
61 (3–1249)
Thorax CT (2–3)
1.0
NT-proBNP,
pg/ml
1
512 (5–25826)
Thorax CT (1–2)
1.0
2
556 (5–10054)
Thorax CT (1–3)
0.12
3
1398 (8–35000)
Thorax CT (2–3)
0.25
Ferritin, ng/ml
1
463 (14–5812)
Thorax CT (1–2)
0.23
2
659 (39–2797)
Thorax CT (1–3)
0.006
3
827 (21–3882)
Thorax CT (2–3)
0.59
D-dimer,
μ
g/l
1
1034 (230–10850) Thorax CT (1–2)
0.66
2
1349 (270–8970) Thorax CT (1–3)
0.005
3
1918 (370–19440) Thorax CT (2–3)
0.20
Procalcitonin,
ng/ml
1
0.21 (0–5.9)
Thorax CT (1–2)
1.0
2
0.25 (0–7.35)
Thorax CT (1–3)
0.01
3
2.03 (0–57)
Thorax CT (2–3)
0.03
CRP, mg/l
1
47 (1–300)
Thorax CT (1–2)
<
0.01
2
84 (3–353)
Thorax CT (1–3)
<
0.01
3
124 (8–460)
Thorax CT (2–3)
<
0.01
Fibrinogen,
mg/dl
1
502 (146–1020)
Thorax CT (1–2)
<
0.01
2
600 (414–1028)
Thorax CT (1–3)
<
0.01
3
593 (294–896)
Thorax CT (2–3)
1.0
Neutrophil,
cells/
μ
l
1
4571 (20–27490) Thorax CT (1–2)
0.11
2
5525 (620–15340) Thorax CT (1–3)
0.01
3
5949 (870–18100) Thorax CT (2–3)
1.0
Lymphocyte,
cells/
μ
l
1
1209 (200–2800) Thorax CT (1–2)
0.48
2
2090 (350–81150) Thorax CT (1–3)
1.0
3
911 (110–3480)
Thorax CT (2–3)
0.36
hs-TNT, high-sensitivity troponin T; NT-proBNP, N-terminal pro-B-type natri-
uretic peptide; CRP, C-reactive protein.



















