
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 2, March/April 2021
AFRICA
109
is present, a sign nowadays rarely searched for, is also proof of
absent atrial contraction. However, in the emergency setting,
a rapid approach to this patient is needed, and diagnosis must
be confirmed with ECG, jugular venous pulse observation and
transthoracic echocardiography, tools readily available in the
majority of emergency departments.
AS can be a serious condition as the loss of active atrial
contraction and profound bradycardia can lead to markedly
decreased cardiac output. Cardiac arrest can also occur, not only
because the escape mechanism can be unstable but also because
the bradycardia can be extreme, and pause-related ventricular
arrhythmias such as polymorphic ventricular tachycardia can
arise.
6
Moreover, blood stasis, originating with no atrial activity,
can cause thromboembolic events, as would happen with other
arrhythmias such as atrial fibrillation.
2,6
Treatment of AS depends on clinical consequences and
the underlying cause. If the patient shows important signs
of heart failure, treatment with diuretics and vasodilators is
indicated, as well as positive chronotropic drug infusion, such as
isoproterenol, for a limited time as a supportive measure while
the underlying condition that gave rise to the AS is corrected.
Temporary transvenous pacing should be deferred and only
used as a last resort if chronotropic drugs are insufficient, in cases
of a high-degree atrioventricular block without escape rhythm,
and for pacing in cases of pause-related ventricular arrhythmias.
Temporary transcutaneous pacing should be avoided, as pacing
provided by patches and an external defibrillator does not
provide reliable ventricular stimulation and should only be used
under strict monitoring when no other option is available.
7
Conclusion
Severe hyperkalaemia in the context of acute kidney injury
was the most likely cause of AS in this case. We highlight
three learning points: (1) AS is an uncommon but potentially
hazardous condition, which can present as a complication of
diabetic ketoacidosis; (2) diagnosis of AS can be made with
readily available tools in any emergency room, such as ECG and
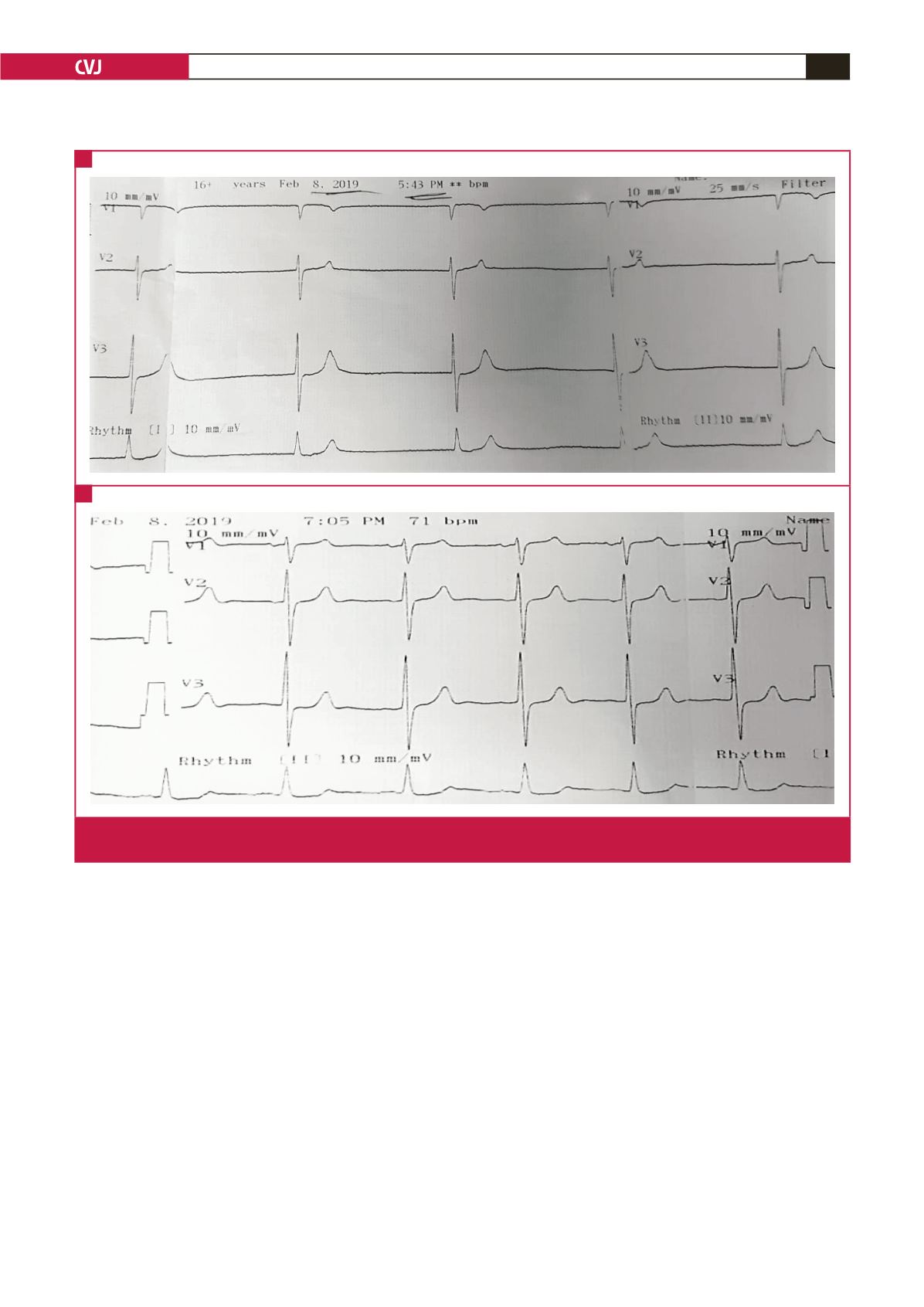
Fig. 1.
A: Initial ECG showing slightly irregular junctional rhythm and absence of atrial electrical activity. B: ECG showing sinus
rhythm after metabolic and electrolyte correction.
A
B



















