
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 2, March/April 2021
AFRICA
103
methods, which usually identify patients with higher burdens of
AT. Moreover, several studies have shown that AHRE do not
seem to be temporally associated with stroke.
15,16
These two main
differences support the idea of two distinct clinical entities.
Incidence and prevalence
The reported incidence of AHRE varies with the definition
of AHRE, study design, indication for CIED, presence of AF
history, following period and type of device.
Because many CIED-recorded arrhythmias have proven to be
inaccurate, the diagnosis of AHRE requires several criteria as
well as manual reviewing of the electrogram (EGM). Therefore,
a > 190-bpm threshold has been chosen to increase the specificity
of CIED-diagnosed AHRE. While this threshold increased the
specificity of the AHRE diagnosis, one study reported that
almost 20% of the CIED-detected AHRE were not accurate
when reviewed by an expert.
17
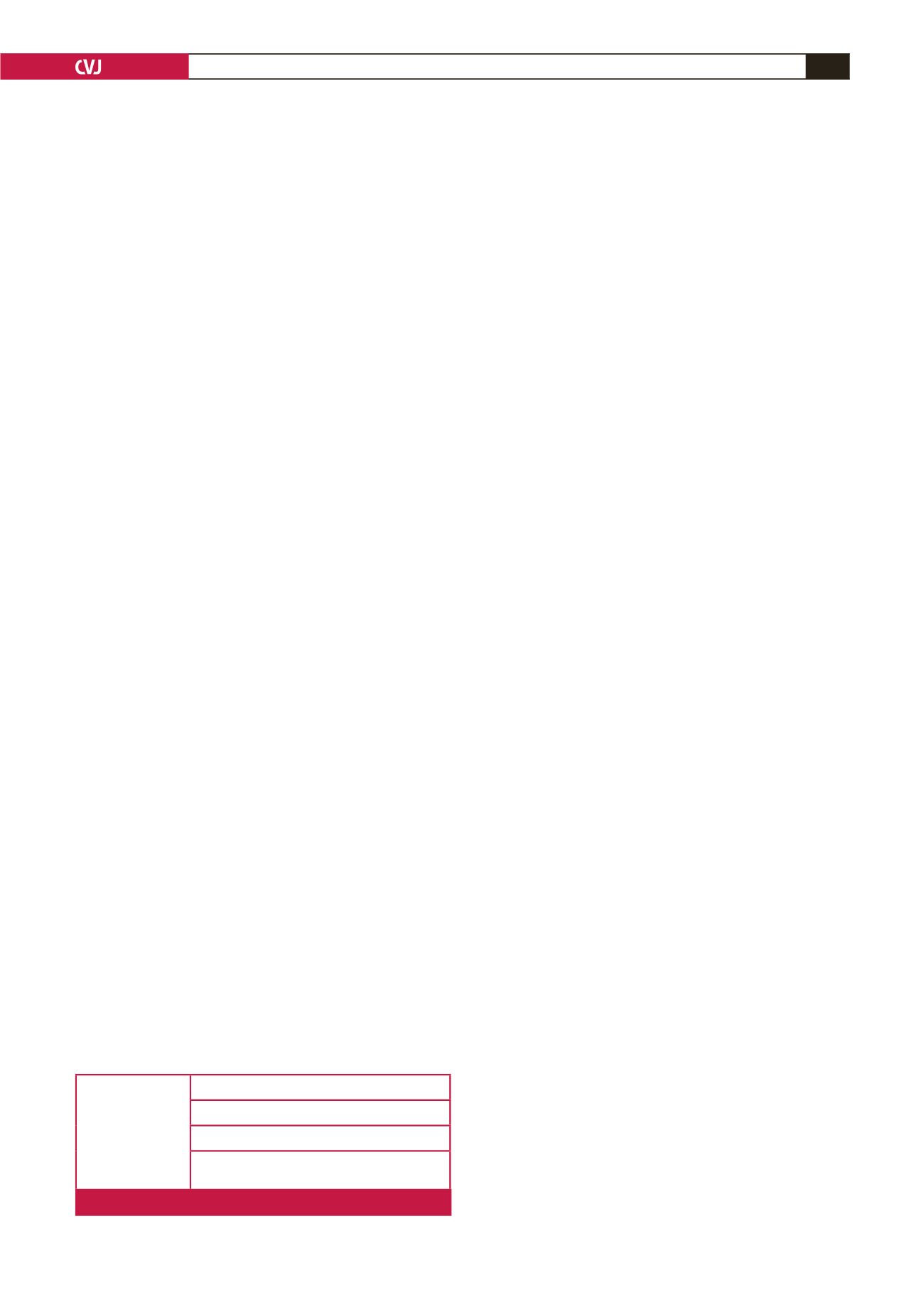
There are a number of different issues why a CIED can
misdiagnose an AHRE episode, which can be classified into
false-negative detection (true atrial undersensing because of
small EGM signals, functional atrial undersensing because of
the EGM signals coinciding with blanking times) and false-
positive detection (myopotential oversensing, electromagnetic
interference and lead failure) (Fig. 1).
12
The specificity of the diagnosis also depends on the type of
device and the duration of the arrhythmic episode. Therefore,
a temporal threshold of five to six minutes was established
for several reasons. First of all, to increase the specificity of
the diagnosis (decrease the number of false-positive detected
episodes).
13,18
Second, episodes longer than five minutes have
been shown to increase the risk of stroke.
13,18
Furthermore,
certain devices were programmed to only record and classify
events longer than a pre-established temporal threshold.
The overall incidence of AHRE in unselected patients is
approximately 50%.
13,19-22
However, the studies that excluded
patients with a history of AF reported an incidence of
approximately 30%.
23-25
The patient population included in most
of the above-mentioned studies consisted of elderly patients
(mean age > 70 years) with multiple thromboembolic risk
factors (mean CHA
2
DS
2
-VASc score > 2).
13,19-25
An atrial lead
is necessary for the CIED in order to accurately diagnose an
atrial arrhythmia, which is why single-chamber CIEDs with a
ventricular lead have not been included in most studies.
Predictive factors
While AF is still a matter of great interest, the underlying
mechanisms that cause and maintain this arrythmia have
not been fully understood. Numerous clinical, biological and
paraclinical factors have been associated with AF but there are
only a handful of studies that examined the role of predictive
factors in AHRE.
In the TRENDS study, the incidence of newly detected
AHRE did not vary with the CHADS
2
score (CHADS
2
score
of 1: 30%, CHADS
2
= 2: 31%, CHADS
2
= 3: 31%) but episodes
longer than six hours were associated with an increased CHADS
2
score.
24
One study, which included patients with a prior history of
AF, showed that older age and increased left atrial volumes were
predictors for pacemaker-detected AF.
20
An increased percentage of ventricular (VVI) pacing has
been associated with an increased risk of developing AF.
26
However, even in patients with dual-chamber pacemakers,
where atrioventricular synchrony is preserved, an increased
percentage of ventricular pacing has been associated with a
higher risk of developing AF.
27-35
The most likely explanation is
that ventricular pacing causes paradoxical septal motion, which
alters interventricular synchrony, lowers ejection fraction and
increases filling pressures in the heart chambers. This leads to
electric remodelling of the left atrium.
Cumulative ventricular pacing of > 50% has been associated
with an increased risk of developing AHRE in patients with no
prior history of AF.
23,36
However, one study showed that a high
percentage of atrial pacing can also be detrimental. In this study,
conducted on patients with no prior history of AF, cumulative
atrial pacing > 50% was associated with a three-fold increase in
risk of developing AHRE.
37
Tekkesin
et al
. demonstrated that inter-atrial block (IAB)
was a predictive factor of AHRE occurrence; 30.1% of the 367
pacemakers implanted for sinus node dysfunction presented
AHRE six months after the implantation, at device interrogation.
Only 67 patients (27%) in the AHRE-negative group presented
with IAB compared to 48 (44.9%) patients in the AHRE-positive
group.
38
Another study conducted by Rubio Campal
et al.
also
found IAB to be a strong predictor for developing AHRE.
39
Although inflammation has been proven to play a certain role
in developing and maintaining AF, the underlying mechanism is
not fully understood.
40-42,43
Pastori
et al.
were the first to associate
inflammation with an increased risk of developing AHRE.
44
The
results showed that high C-reactive protein and white blood cell
count were independently associated with AHRE occurrence.
These results suggest a common pathogenetic pathway between
AF and AHRE. Another interesting finding of this study was
that there was no association between anti-arrhythmic treatment
and AHRE incidence, which implies that an optimal level for the
management of this arrythmia has not yet been reached.
44
AF can be a marker of underlying vascular disease because
of the direct and indirect mechanisms leading to electrical and
anatomical atrial remodelling, which lead to atrial fibrosis.
42,45
The prevalence of CAD in patients with AF ranges from 17 to
46.5%.
46-48
The relationship between vascular disease and AHRE
has not been sufficiently investigated. More studies are necessary
to investigate the underlying mechanisms and predictive factors
of AHRE.
Clinical impact
Atrial high-rate episodes must be distinguished from clinical
AF, which is diagnosed by surface ECG and identifies patients
with a higher burden of AF. The ancillary MOST analysis was
the first study to prove that in CIED patients, AHRE of more
False-positive
AHRE
Myopotential oversensing
Electromognetic interference
Lead failure
Ineffective atrial pacing
(non-re-entrant VA synhrony)
Fig. 1.
Causes for incorrect AHRE detection by the CIED.



















