CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 3, May/June 2011
144
AFRICA
the ascending aorta. Therefore traumatic pseudoaneurysm asso-
ciated with insertion of the tube was excluded (Fig. 2). It was
thought that the pseudoaneurysm was associated with contami-
nation with purulent bacterial effusion. Because of the risk of
spontaneous rupture, emergency surgery was performed via a
sternotomy using cardiopulmonary bypass.
The mycotic pseudoaneurysm of the ascending aorta arose
from the postero-lateral wall of the aorta above the sinotubular
junction. The aortic wall defect left by the neck of the pseu-
doaneurysm was about 3
×
4 cm after excision of the pseodo-
aneurysm. The defect margins were reached between the non-
coronary and left coronary cuspis commissures. The aortic wall
defect was closed with a pericardial patch, with the use of 4/0
polypropylene sutures together with non-coronary commissural
resuspention stitch.
The patient had an uneventful postoperative recovery. MSCT
was repeated postoperatively and showed no pathology relating
to the ascending aorta and no pseudoaneurysm (Fig. 1D).
Conclusion
We reported on a child with a normal cardiac history who had
developed a mycotic pseudoaneurysm of the ascending aorta due
to purulent bacterial pericardial effusion in the absence of aortic
surgery or blunt trauma.
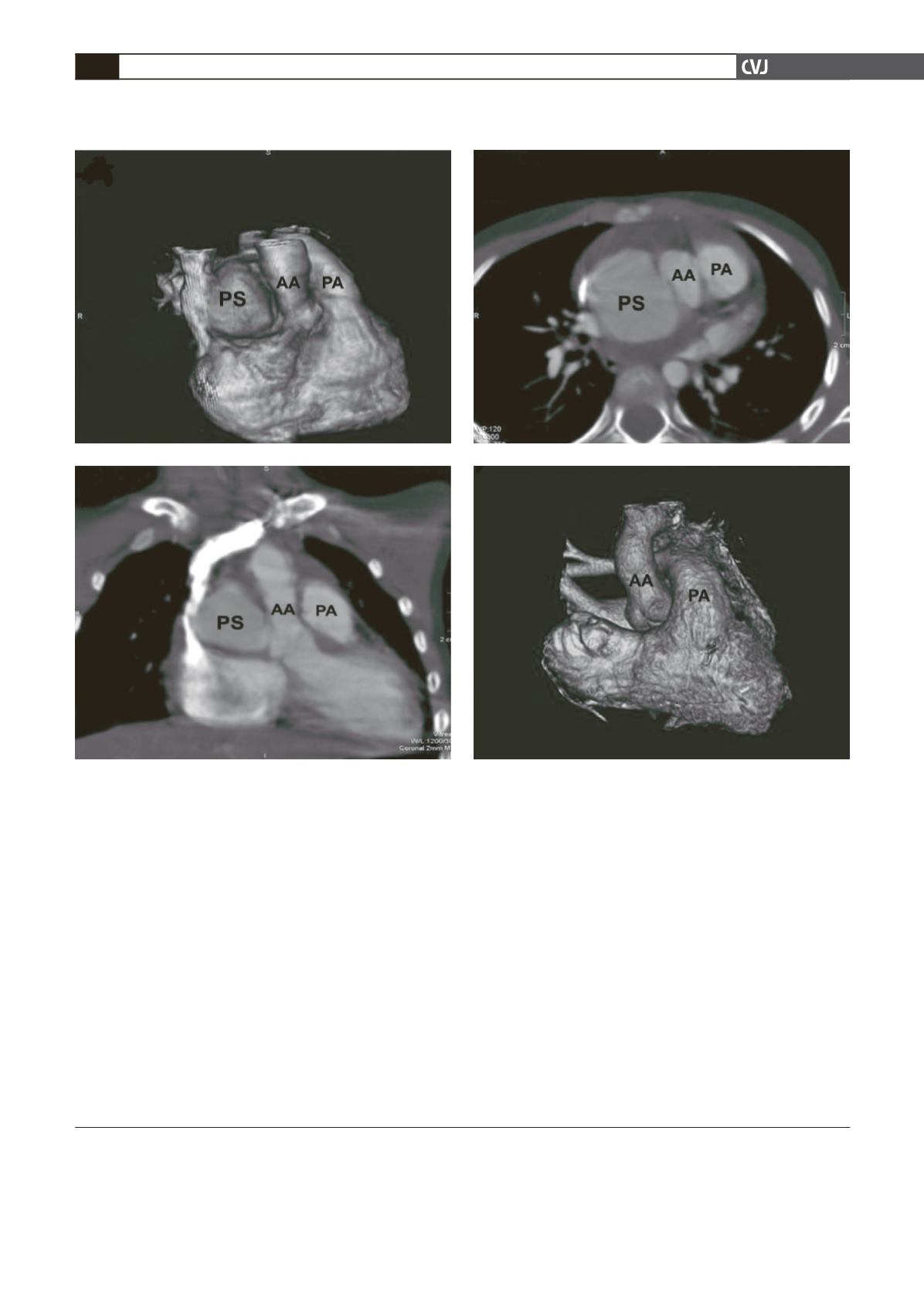
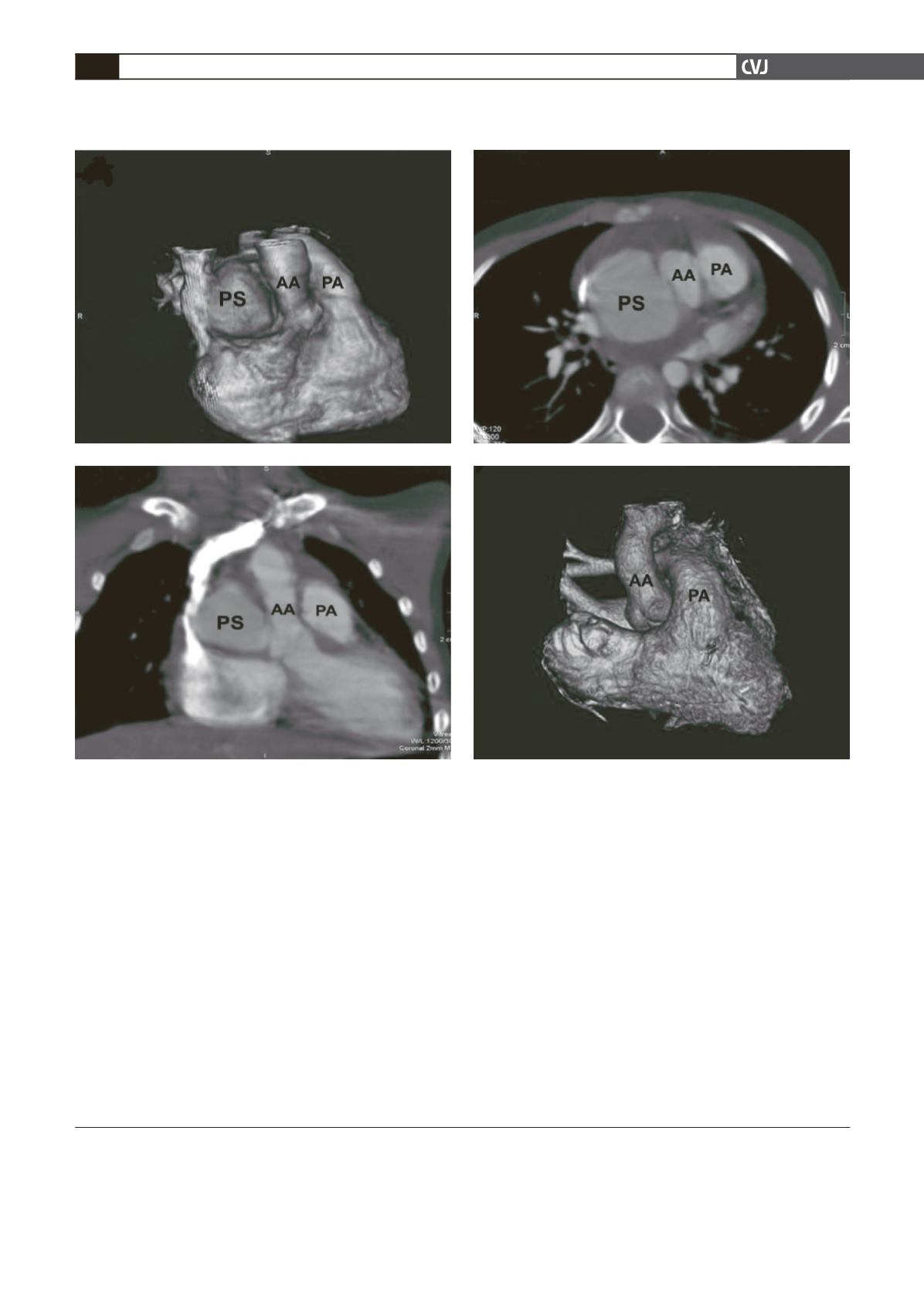
Fig. 1A–C: Multi-slice computed tomography showing a 4 × 5-cm mass between the superior vena cava and ascending
aorta, which was diagnosed as a pseudoaneurysm. D: Postoperatively, multi-slice computed tomography showed no
pathology relating to the ascending aorta and no pseudoaneurysm.
C
D
A
B