CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 2, March/April 2014
AFRICA
53
six HIV-infected patients with pericardial effusion had severe
valvular regurgitation, two with heart failure and fluid overload,
and none had impaired systolic function.
HIV stage and echocardiographic features
The mean CD
4
count in the HIV-infected patients was
189 /mm³. To determine any association with the stage of
immunodeficiency, the echocardiographic findings were
examined in the HIV-infected patients and stratified into two
groups: CD
4
counts
<
200 /mm³ and
>
200 /mm³. No striking
differences emerged between the groups in vegetation size and
number of valves affected, complication rate, organism, ejection
fraction or outcome.
Three of the four patients with leaflet aneurysms, and all of
those with aortic root abscess had CD
4
counts
<
250 /mm³. The
four patients with
S aureus
infection all had CD
4
counts
<
250 /
mm³ (248, 231, 149 and 139 /mm³). Three of the four patients
with very low CD
4
counts (
<
100 /mm³) had vegetations, and the
fourth had an aortic root abscess without vegetations.
Surgical findings
In all patients, medical therapy with appropriate antibiotics
had been instituted and continued for a total period of six
weeks. Forty patients (34 HIV uninfected and six HIV infected)
underwent valve-replacement surgery. At surgery, the underlying
valve pathology was considered to be rheumatic in origin in 38
cases (95%). In the two remaining cases, the underlying valve
was considered normal by the operating surgeon. Among the
six HIV-infected cases, surgery revealed underlying rheumatic
valve pathology in five patients; in the remaining patient the
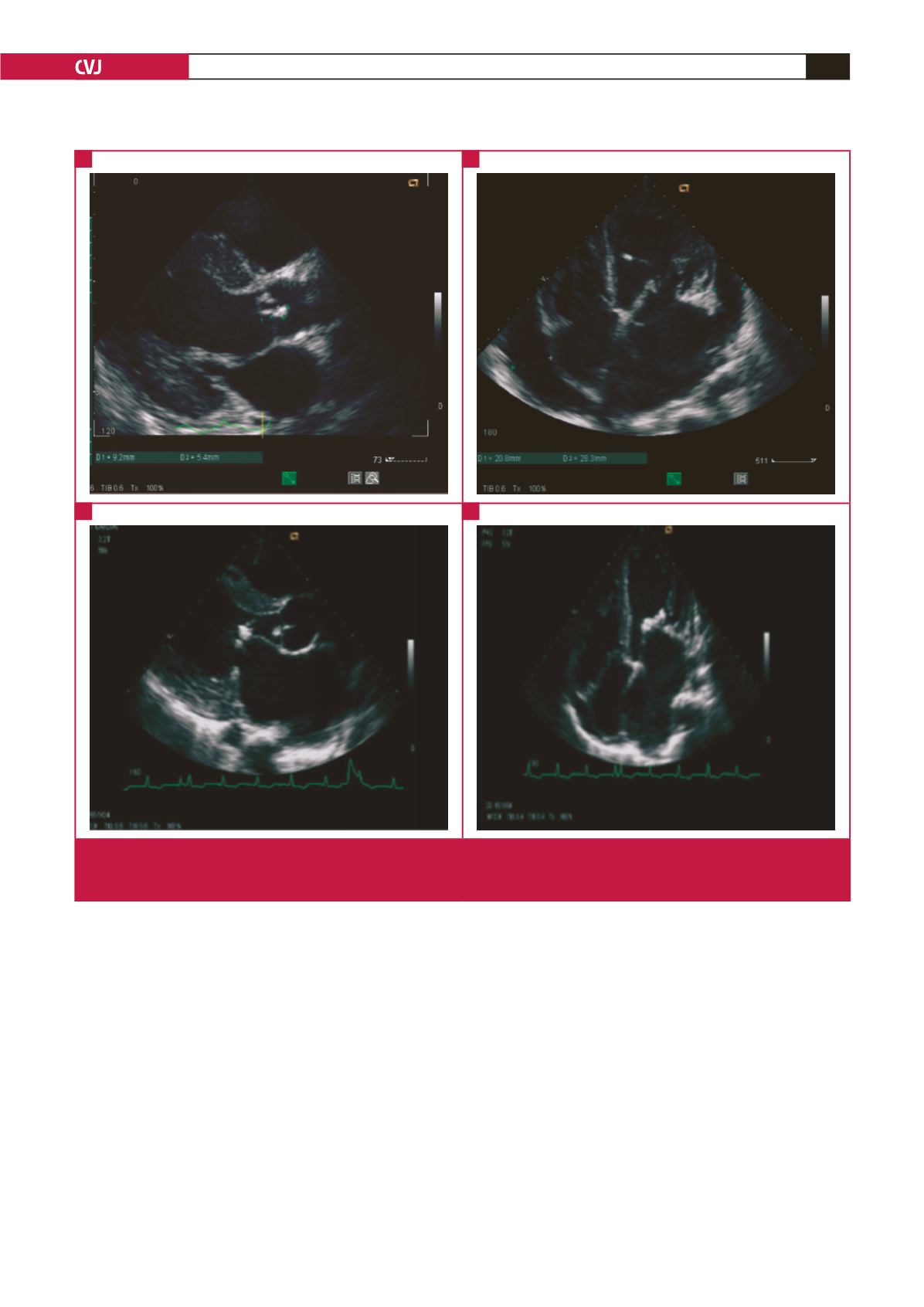
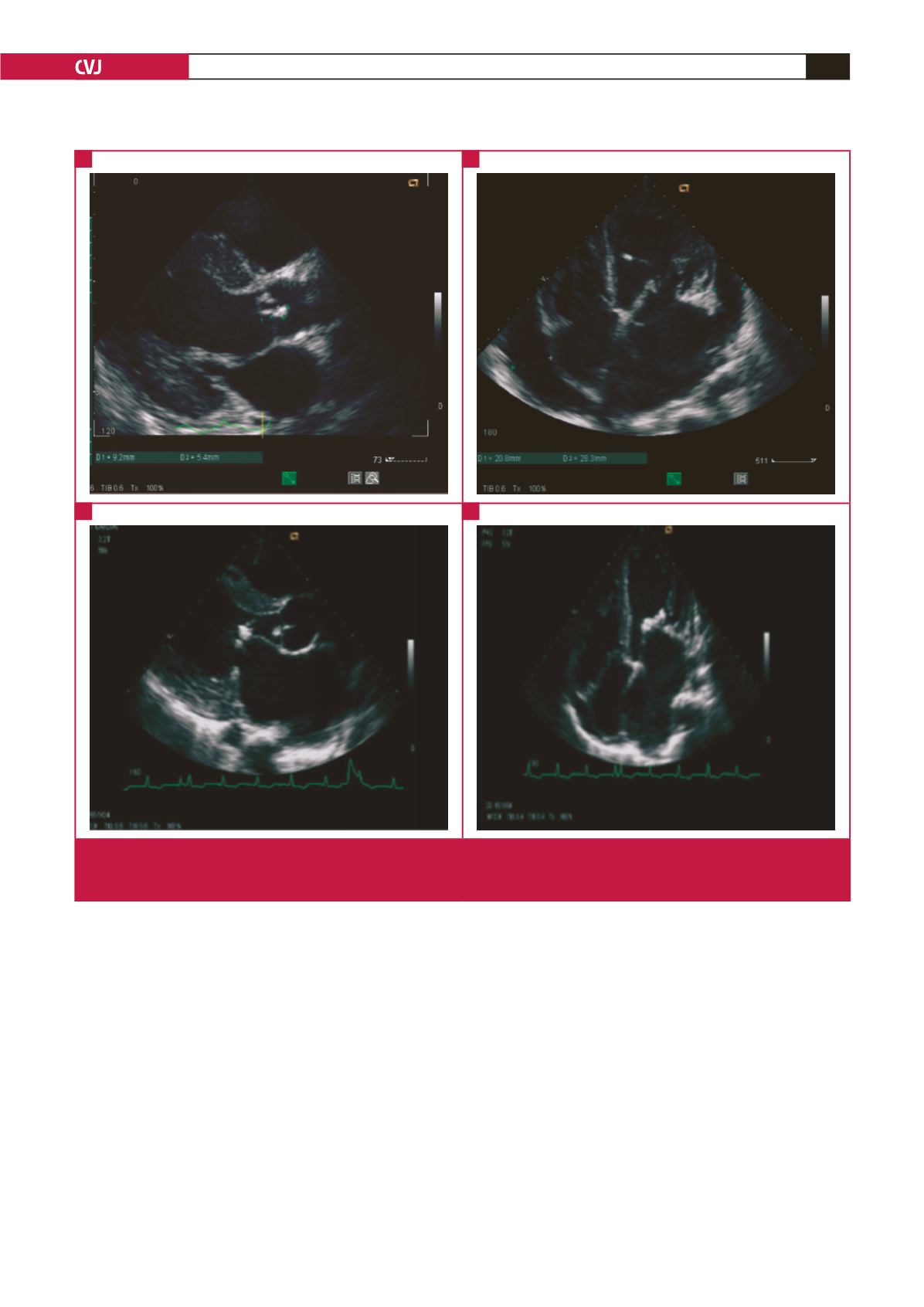
Fig. 1.
Vegetations on the aortic valve (parasternal long-axis view) (A), and on the mitral valve chord (apical four-chamber view)
(B), in an HIV-positive patient. Vegetations on the aortic valve (parasternal long-axis view) (C), and mitral valve (apical four-
chamber view) (D), in a HIV-negative patient.
A
C
B
D