CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 3, May/June 2014
AFRICA
125
factors and accompanying vascular or non-vascular diseases.
An arterial examination of the lower extremity, and an ankle/
brachial pressure index (ABI) and arterial duplex examination of
the patients were then performed.
Patients with ASO who matched the criteria for inclusion in
this study were those with atherosclerotic lower limb ischaemia
at the time of admission, and patients with lower extremity
involvement. Patients with Buerger’s disease who matched
the criteria for inclusion in this study were those with lower
extremity involvement, and patients with Buerger’s disease,
diagnosed according to Shionoya’s criteria,
4
at the time of
admission. These criteria included smoking history; onset before
the age of 50 years; infra-popliteal arterial occlusions; either
upper limb involvement or phlebitis migrans; and absence of
atherosclerotic risk factors other than smoking. Written informed
consent was obtained from all study participants.
At the time of hospital admission, the patients’ ischaemia was
evaluated according to the clinical categories of chronic limb
ischaemia (Rutherford classification
5
) by inviting patients back
to the hospital at six and 12 months following the first admission.
Patients’ quality of life was evaluated from the Short Form
Health Status Survey (SF-36), which provides a measurement
of change in physical components, including physical function,
physical status, bodily pain and general health, as well as mental
components, including mental health, emotional status, social
function and vitality.
The impact of PAD was also evaluated from the Vascular
Quality-of-Life Questionnaire (VASCUQOL), which consists of
pain, symptoms, activities, social well-being and emotional well-
being domains.
6
The questionnaries were applied by a research
staff member who had no information on these patients.
Following the measurement of quality of life, treatment
modalities including surgery or medical therapy, where necessary
and appropriate, were initiated. In general, endovascular and
bypass procedures were preferred for ASO patients with critical
ischaemia and unbearable claudication. Risk-factor reduction
and medical treatments were used for all ASO patients. For
Buerger’s disease patients with critical ischaemia, the target
vessel was evaluated for distal bypass and smoking cessation was
advised. Distal bypass was used for patients where appropriate.
Sympathectomy, infusion of prostaglandin (PGE2), medical
treatment and wound care were used for patients in whom distal
bypass was inappropriate or in those who had failed bypass.
In the presence of necrotic tissue, minor or major amputations
were performed. All parameters evaluated at baseline were also
repeated at six and 12 months post admission.
Statistical analysis
Comparisons between groups were made using Pearson’s
chi-square test for categorical variables and independent
t
-tests
for continuous variables. A
p
-value less than 0.05 was accepted
as statistically significant. Statistical analyses were carried out
using SPSS for Windows 15.0 (SPSS Inc., Chicago, Illinois,
USA).
Results
A total of 86 patients, 47 with ASO and 39 with Buerger’s
disease, were included in the study. Demographic characteristics
and additional diseases at the time of admission of the patients
are shown in Table 1. The rate of smoking was statistically
significantly higher in Buerger’s disease patients than in
those with ASO (
p
=
0.002). The frequency of diabetes and
hypertension was significantly higher in ASO patients than in
those with Buerger’s disease (
p
<
0.001,
p
<
0.001 respectively).
Vascular involvement at the time of admission
In the ASO group, claudication was identified in 23 (48.9%)
patients, pain at rest occurred in six (12.8%), and ischaemic
wound symptoms were observed in 18 (38.3%) patients. In
the Buerger’s disease group, claudication was identified in
one (2.6%) patient, pain at rest occurred in six (15.4%), and
ischaemic wound symptoms were observed in 32 (82%) patients
at the time of admission to hospital. The rate of ischaemic wound
symptoms in patients with Buerger’s disease was statistically
significantly higher than in the ASO group (
p
=
0.001).
There were statistically significant differences between the
groups in anatomical localisation of ischaemic wounds, which
were determined with invasive and non-invasive methods. In
Buerger’s disease patients, the level of disease was observed to
be mostly at the popliteo-crural level. In the ASO group, aorto-
iliac involvement was present in 18 (38.2%) patients, femoro-
popliteal involvement was found in 18 (38.2%), and popliteo-
crural involvement was present in 11 (23.4%) patients. In the
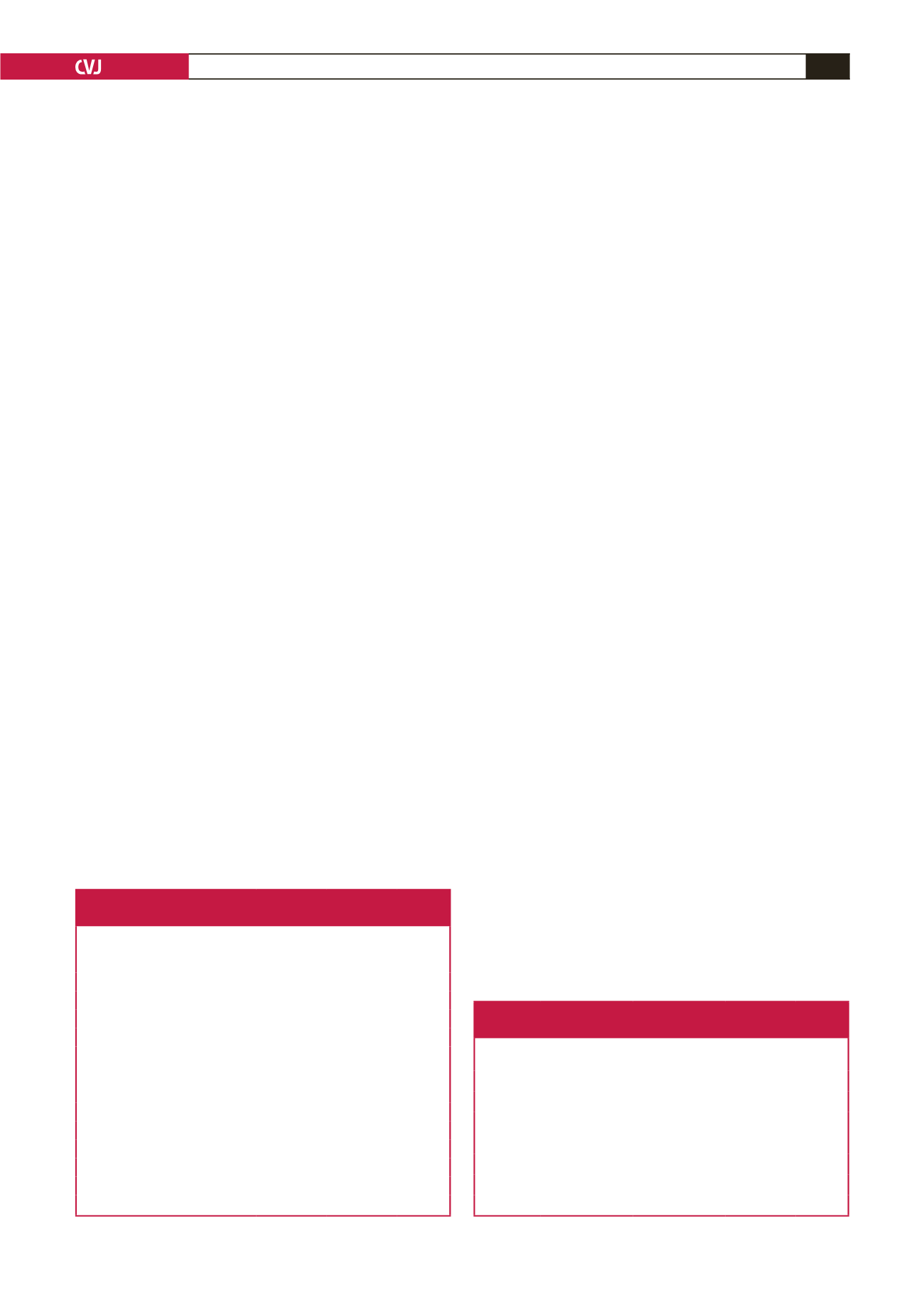
Table 1. Demographic characteristics, additional diseases
and amputation rates of patients
Athero-
sclerosis
(
n
=
47)
Buerger’s
disease
(
n
=
39)
p
-value
Age (years)
60.28
47.77
ns
Gender
Male (%)
80.9
94.9
ns
Female (%)
19.1
5.1
ns
Smoker (%)
59.6
94.9
0.002*
Non-smoker (%)
40.4
5.1
ns
Additional diseases
Diabetes (%)
49.1
9.6
<
0.001*
Hypertension (%)
49.9
7.6
<
0.001*
Obesity (%)
4.4
5.4
ns
ABI (mean)
0.42
0.40
ns
Affected extremity (right–left) (%)
51–41
25–41
ns
ABI = ankle/brachial pressure index. *Statistically significant value.
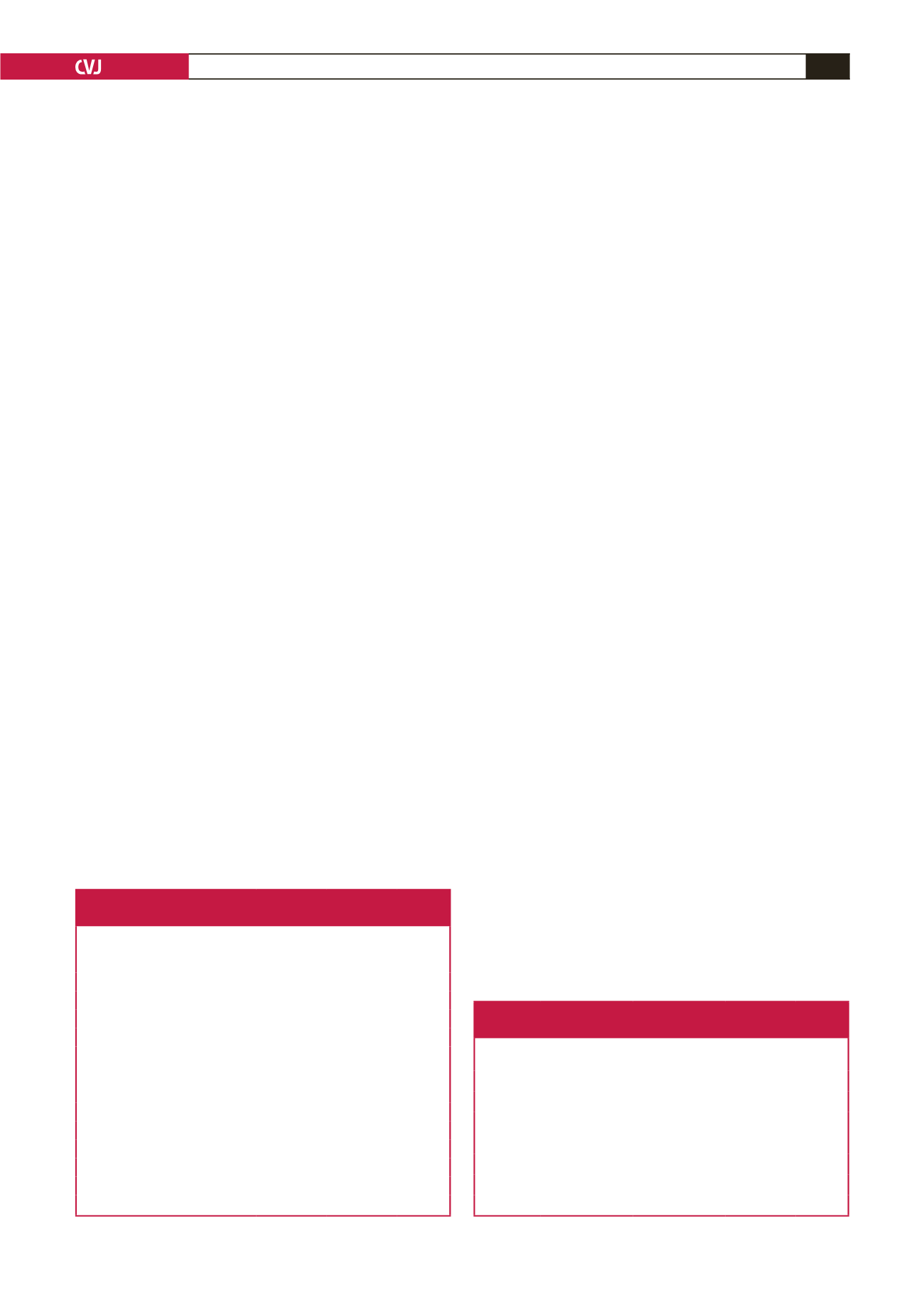
Table 2. Comparison of the two groups in terms of chronic
limb ischaemia criteria
Category
Atherosclerosis,
n
(%)
Buerger’s
disease,
n
(%) Total,
n
(%)
p
-value
Category 1
2 (4.3)
0 (0)
2 (2.3)
ns
Category 2
9 (19.1)
0 (0)
9 (10.5)
ns
Category 3 12 (25.5)
1 (2.6)
13 (15.1)
ns
Category 4
6 (12.8)
6 (15.4)
12 (14)
ns
Category 5 18 (38.3)
30 (76.9)
48 (55.8)
<
0.001*
Category 6
0 (0)
2 (5.1)
2 (2.3)
ns
*Statistically significant value.