CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 3, May/June 2014
116
AFRICA
it was 2.2
±
0.03 (
p
<
0.05). The pulmonary arterial pressure
(PAP) ratio in the device group was 28.2
±
1.34 mmHg and in
the surgery group it was 33.8
±
0.89 mmHg (
p
=
0.01). The mean
length of hospital stay in the device group was 1.92
±
0.43 days
and in the surgery group, 7.14
±
0.14 days (
p
<
0.05).
Follow up was available for 42 (46%) patients in the device
group and for 121 (87%) in the surgery group. During the
follow-up period, complete closure was observed in 41 of 42
patients (97.6%) in the device group and in all 121 patients in the
surgery group (100%) (
p
=
0.258). In one patient (3%), a small
(
<
2 mm wide) colour jet residual shunt as assessed by colour
Doppler echocardiography in the device group and the patient
was followed up without additional processing.
Cardiac arrhythmias requiring pacemaker placement or long-
term anti-arrhythmia medication were not observed. Minor
cardiac arrhythmias not requiring medical treatment in hospital
were observed in one patient in the device group (3%) (first-
degree AV block), and in three patients in the surgery group (2%)
(two with sinus arrhythmia and one with first-degree AV block)
(
p
=
0.72). During the three-month follow up, arrhythmias were
not observed in either group (
χ
2
=
0.0,
p
=
0.0).
The mean amount of mediastinal bleeding was 364
±
19.6
ml, and moderate bleeding was observed in two patients (1.5%).
These patients in the surgery group underwent revision surgery
for bleeding. Pericardial effusion due to surgery was observed in
four patients (3.3%) and treated with medical therapy. Infection
of the surgical site was not observed, while pulmonary infections
were observed in two patients (1.5%) in the surgery group.
Haematoma in the femoral region was observed in four patients
(9%) in the device group.
None of the patients experienced worsening related to
mitral or tricuspid valve regurgitation, and none developed
left ventricular failure in either group. There were no cases
of erosions, ischaemic stroke, cardiac perforation, late
embolisation, thrombus formation, or malposition of the device
after percutaneous closure of the ASD. Mortality was 0% for
both groups. Complications and outcomes of the patients are
given in Table 2.
Discussion
Transcatheter closure of ASD with septal occluder devices has
increasingly become a practical alternative to surgical techniques
in patients with suitable ASDs. Its principal benefits include
fewer complications, the absence of an incision scar, shorter
length of hospital stay and less discomfort for the patients. The
efficacy of percutaneous device closure has been well reported
from case series and comparative studies.
2-5
Our study confirms previous findings that ASD closure is
generally successful and involves low morbidity and mortality
rates with both surgical and device closure.
5-8
In some series,
6,7
complete closure (with no residual shunt) was achieved less
often by the percutaneous method. In our study, however, as in
other series, the success rate was similar for both techniques.
Complication rates with either treatment modalities were
reported to be low.
5-8
The most frequently reported complications
after surgical closure were arrhythmia, pericardial effusion,
mediastinal bleeding needing revision, and infection, together
with the potential risks associated with blood transfusion. On the
other hand, device closure may be accompanied by tamponade,
embolisation of the device, symptomatic gaseous embolism, or
unwanted problems related to femoral puncture.
1,5,9
In the device group, femoral haematoma was observed in four
patients in our study. There was no case of thrombus-related
embolism or cardiac tamponade. However complications,
although minor, occurred more frequently in the surgery group.
There were four cases of pericardial effusions in this group.
Length of hospital stay was significantly longer in the surgery
group, which is in agreement with other comparative studies.
5-8
Apart from the length of hospitalisation, the groups were
comparable, with good cardiac outcomes.
Another important consideration favouring device closure
is the absence of a surgical scar. This is a notable advantage,
particularly in female patients. Parallel with improvements in
closure device technology, there have also been improvements
in the surgical approach, such as using mini-sternotomy,
thoracotomy, and endoscopic and robotic surgery.
10-12
Although
we usually use the minimally invasive approach, due to the
patient numbers in our surgical group, we performed only a
standard sternotomy. Our results are comparable with the device
group, with good outcomes.
There were some limitations to this study. It had a retrospective
design and patient groups were non-randomised. Only 71%
of patients had complete sets of data. In retrospective studies,
managing to collect full sets of data is difficult. Additional
studies and longer-term follow up of these or other randomised
patient groups would be valuable for making recommendations
about treatment modalities.
Conclusion
There have recently been dramatic developments in both surgical
and percutaneous methods of treatment of ASDs, together with
the development of emerging technologies. New strategies
are an improvement on older methods and device closure is
replacing open-heart surgery, especially in suitable patients with
isolated ASDs. The range of indications for device closure is
frequently not well defined. Increasing the range of indications
for device closure, however, may cause complications that
would make surgical treatment a more attractive option. As is
evident from this study, surgical treatment can be performed
efficaciously with low complication and mortality rates. The
surgical approach therefore maintains its position as an essential
alternative method, particularly in patients who are unsuitable
for device closure.
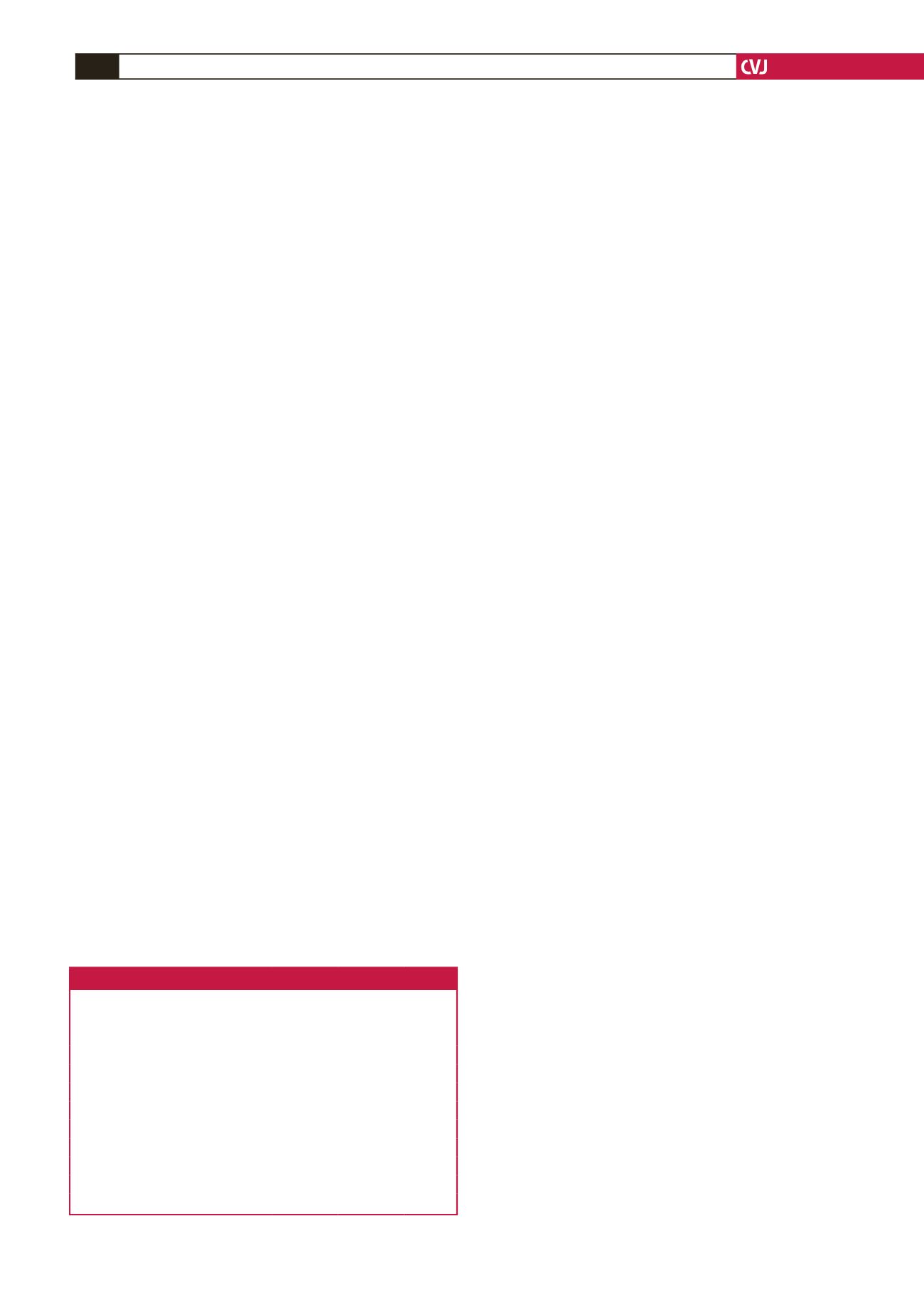
Table 2. Complications and outcomes during follow up.
Device
Surgery
p-
value
Residual shunt,
n
(%)
1 (2.4)
0
0.258
Moderate bleeding and revision,
n
(%)
–
2 (1.7)
Pulmonary infection,
n
(%)
0
2 (1.7)
Surgery site infection
–
0
Arrhythmias in hospital,
n
(%)
1 (2.4)
3 (2.5)
0.726
Arrhythmias during follow up
0
0
Mean hospital stay (days)
1.92
±
0.43 7.14
±
0.14
<
0.001*
Mean mediastinal drainage (ml)
–
364
±
19.6
Pericardial effusion,
n
(%)
–
4 (3.3)
Femoral haematoma,
n
(%)
4 (9)
–
*Independent samples
t-
test.