CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 6, November/December 2014
280
AFRICA
the end of the cardiopulmonary bypass. Nasal wet oxygen
therapy (2–4 l/min) was initiated in all patients after extubation.
Aspirin treatment (300 mg/day) was started after mediastinal
bleeding had ceased in all patients. Hypertension was diagnosed
if the systolic blood pressure (BP) was above 140 mmHg or
diastolic BP was above 90 mmHg on two or more occasions.
Postoperative records up to discharge from hospital and
available results related to the end-points were compared.
The primary end-point was spontaneous epistaxis (with ENT
consultation), requiring at least one nasal packing after CABG
surgery, and any complications related to nosebleed and
treatment, excluding death. The secondary end-point was death
related to epistaxis.
Statistical analysis
All available data were analysed with the computer program
SPSS (Statistical Package for Social Sciences) for Windows 17.0
(Chicago, IL, USA). Descriptive statistical methods (number,
percentage, mean, standard deviation) were used. Differences in
variables were analysed using the Mann–Whitney
U
, Kruskal–
Wallis and chi-square tests as appropriate, and
p
-values of less
than 0.05 were considered significant.
Results
A total of 27 patients with epistaxis consulted at the
ENT Department. One patient had a history of epistaxis
pre-operatively. There were 19 males (70 %) and eight females
(30%), and their ages ranged between 52 and 72 years (mean 61
±
5); 55% had hypertension, 78% COPD, 48% diabetes mellitus
and 63% a history of smoking.
The overall duration of hospital stay ranged from six to 11
days (mean 7.9
±
1.1) (Tables 1–3). Epistaxis was seen specifically
on the fourth and seventh days postoperatively. Two patients had
two or more epistaxis episodes within 15 days of discharge from
hospital. According to the degree of bleeding, group 1 patients
(
n
=
17, 63%) were treated with anterior, posterior, or anterior
and posterior nasal packing. Group 2 patients (
n
=
6, 22%) were
treated by electrocautery. Group 3 patients (
n
=
4, 15%) were
treated by surgical ligation of the bleeding vessels and blood
transfusions. These four patients in group 3 had two risk factors:
hypertension and COPD (Table 2).
All pre-operative patient characteristics and co-morbid
factors between the groups were similar (
p
> 0.05) (Tables 1–3).
Although all patients with epistaxis presented with discomfort
in the postoperative period, all patients (100%) had a good
recovery with no mortality. Group 3 patients had profuse nasal
bleeding that needed surgical intervention, and both COPD and
hypertension were diagnosed in all four of these patients.
Discussion
Epistaxis is classified on the basis of the primary bleeding
site being anterior or posterior. A common source of anterior
epistaxis is the Kiesselbach plexus, an anastomotic network of
vessels on the anterior portion of the nasal septum. Posterior
bleeding occurs mainly from the branches of the sphenopalatine
artery in the posterior nasal cavity or nasopharynx.
5
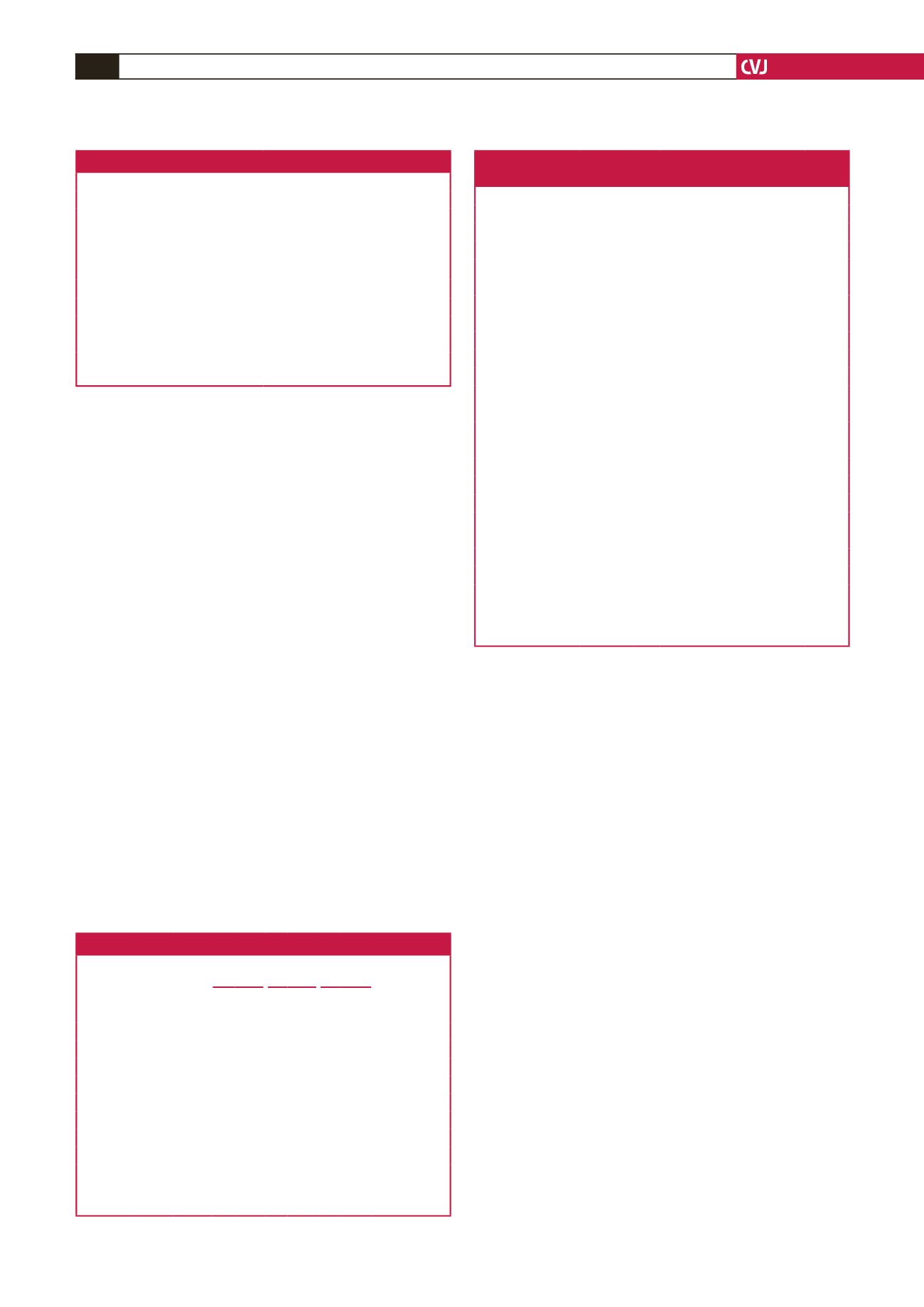
Table 2. Demographics and patient data
Total
number
(%)
Group 1 Group 2 Group 3
p
χ
2
n % n % n %
Gender
27 Female 5 62.5 2 25.0 1 12.5 0.960 0.081
Male 12 63.2 4 21.1 3 15.8
Smoking 17
(62.9)
No 6 60.0 3 30.0 1 10.0 0.704 0.703
Yes 11 64.7 3 17.6 3 17.6
Diabetes
mellitus
13
(48.1)
No 8 57.1 4 28.6 2 14.3 0.708 0.689
Yes 9 69.2 2 15.4 2 15.4
Hyper-
tension
15
(55.5)
No 9 75.0 3 25.0 0 0.0 0.152 3.772
Yes 8 53.3 3 20.0 4 26.7
COPD 21
(77.7)
No 5 83.3 1 16.7 0 0.0 0.415 1.758
Yes 12 57.1 5 23.8 4 19.0
*Statistical significance was established as
p
< 0 .05.
COPD: chronic obstructive pulmonary disease.
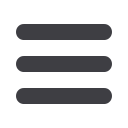
Table 1. Pre-operative patient characteristics
Male/female
19/8
Age (years),
n
(mean)
52–72 (61
±
5.09)
Body mass index (kg/m
2
)
27.55
±
1.36
Smoking,
n
(%)
17/27 (63)
Diabetes mellitus,
n
(%)
13/27 (48.1)
Hypertension,
n
(%)
15/27 (55.6)
aPTT (s)
31
±
2.801
INR
1.107
±
0.1107
Platelet count (/µl)
274444.44
±
74644.456
LVEF (%)
55.05
±
3.79
aPTT: activated partial thromboplastin time, INR: international
normalised ratio, LVEF: left ventricular ejection fraction.
Table 3. Patient characteristics and haematological
parameters in the three groups
Variables
Group n
Mean
±
SD
KW
Age
Group 1 17
61.760
±
5.391
0.696
Group 2 6
60.170
±
4.708
Group 3 4
59.500
±
5.000
Hospital stay
(days)
Group 1 17
7.470
±
0.717
11.469
Group 2 6
8.170
±
1.169
Group 3 4
9.750
±
0.957
BSA (kg/m
2
)
Group 1 17
27.235
±
1.427
2.454
Group 2 6
28.033
±
1.155
Group 3 4
28.200
±
1.178
LEVF (%)
Group 1 17
54.940
±
3.944
0.400
Group 2 6
56.170
±
3.061
Group 3 4
55.750
±
5.439
Platelet count
(per µl)
Group 1 17 252 352.940
±
68 786.755 3.963
Group 2 6 320 000.000
±
56 213.877
Group 3 4 300 000.000
±
100 000.000
aPTT (s)
Group 1 17
30.530
±
2.718
3.217
Group 2 6
30.830
±
3.251
Group 3 4
33.250
±
1.708
INR
Group 1 17
1.100
±
0.117
0.371
Group 2 6
1.133
±
0.121
Group 3 4
1.100
±
0.082
*Statistical significance was established
p
< 0 .05
BSA: body surface area, LVEF: left ventricular ejection fraction,
aPTT: activated partial thromboplastin time, INR: international
normalised ratio.



















