
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 2, March/April 2015
AFRICA
97
episodes of supraventricular tachycardia of unknown origin with
almost daily palpitations on minimal effort. At that time she was
diagnosed with NYHA functional class II failure off medication
(she was not on any medication at presentation). Her mother
had sarcoidosis. Her obstetric history included two threatened
miscarriages and two viable births, both vaginal delivery.
Physical examination was normal and her heart rate was 78
bpm. Holter monitoring did not identify ventricular tachycardia.
Echocardiography revealed a speckled pattern at the basal
segment of the septum and right ventricular wall, suspicious
for an infiltrative disease. Left ventricular function was good
(LVEF 53%) and no valve dysfunction was observed. In view
of the clinical history, those features were highly suggestive of
sarcoidosis with cardiac involvement. Verapamil 40 mg daily was
started and MRI investigation was booked after pregnancy for
further investigation.
One month later she presented with increased palpitations on
verapamil. She had previously responded to verapamil but did
not respond on atenolol or propanolol. The palpitations started
without any obvious trigger and lasted one hour. Haemoglobin
was 11.7 g/dl (normal range, non-pregnant woman: 12.0–15.5
g/dl) and thyroid stimulating hormone was 1.29 mU/l (normal
range: 0.34–4.25 mU/l). She had normal electrocardiography.
Verapamil dosage was increased to 80 mg because of the
increased complaints of palpitations.
At 30 weeks of pregnancy, she presented at the clinic with
daily palpitations and shortness of breath. The palpitations
did not improve on verapamil. Her blood pressure was 108/58
mmHg, she had a regular heart rate of 104 bpm (sinus rhythm)
and was not in congestive heart failure. At that time verapamil
was stopped due to its possible side effects on the foetus.
She delivered at 36 weeks of gestation by emergency caesarean
section due to foetal distress. She gave birth to a healthy male
baby of 2 760 g. Echocardiography was repeated three months
postpartum and demonstrated a speckled pattern, diastolic left
ventricular dysfunction with right ventricular function of 50%
and left ventricular function of 68%.
MRI was performed four months after delivery and showed
a mildly enlarged left ventricle, reduced LVEF (
<
50%) but no
regional wall motion abnormality. The delayed gadolinium
sequences showed basal and mid-ventricular mesocardial and
epicardial enhancement (Fig. 3). The radiologist concluded that
these features could be consistent with sarcoid-related myocardial
scarring. The patient declined to have a transbronchial biopsy.
After starting steroid therapy, there was a marked improvement
in her symptoms, including shortness of breath. The cardiac MRI
was repeated and showed a marked increase in LVEF (from
<
50%
before starting steriod therapy to 70% after starting the therapy).
Discussion
Our cases demonstrate that cardiac sarcoidosis may manifest for
the first time during pregnancy. Reports on cardiac sarcoidosis
related to pregnancy are rare.
1,2
Cardiac sarcoidosis, a potentially
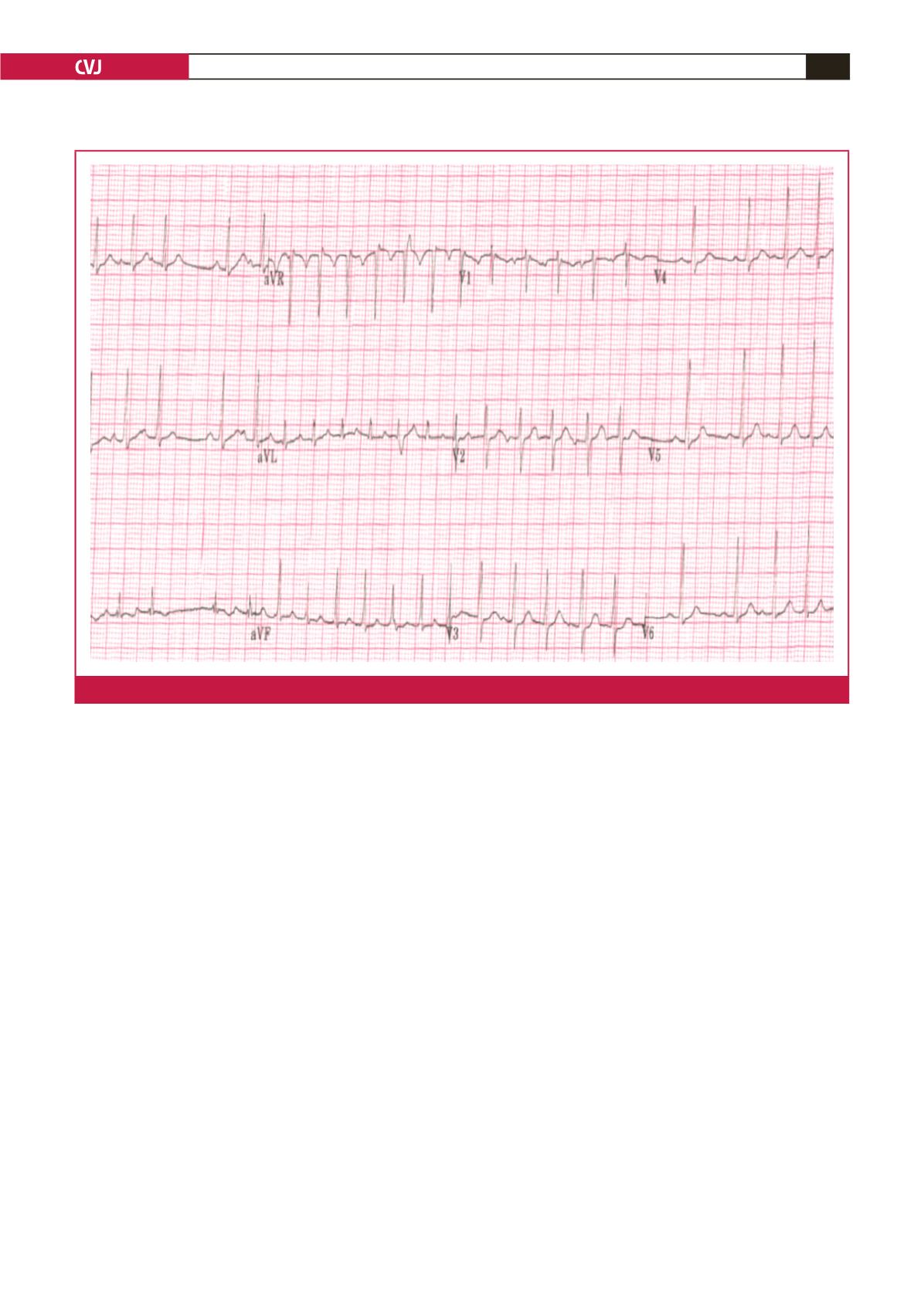
Fig. 1.
ECG of case 1, performed when the patient was 16 weeks pregnant, showing intermittent atrial fibrillation.

















