
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 3, May/June 2015
AFRICA
141
The average haemoglobin levels were 9.4
±
1.8 and 13.8
±
4.9 g/l
in the anaemic (A) and non-anaemic (NA) patients, respectively
(
p
=
0.0001). The main patient characteristics are shown in
Table 1.
Heart failure was biventricular in 233 cases (85.7%) and
left HF in 39 cases (14.3%). Two hundred and forty-nine
patients (91.5%) were in NYHA functional class III–IV, with no
difference between the A and NA patients (
p
=
0.6). The heart
diseases diagnosed were hypertensive heart disease in 106 cases
(39.0%), dilated cardiomyopathy in 86 cases (31.6%), myocarditis
in 27 cases (9.9%), valvular heart disease in 24 cases (8.8%),
ischaemic heart disease in 15 cases (5.5%), and unspecified cause
in 14 cases (5.1%).
Average left ventricular ejection fraction was 48
±
14.6% in A
and 51.3
±
15% in NA patients (
p
=
0.43
). Average glomerular
filtration rate was 54.6
±
12.5 ml/min in A and 70.4
±
10.2 ml/min
in NA patients (
p
=
0.004). Forty-seven patients (17.3%) were on
oral anticoagulation and 15 (5.5%) were on aspirin.
The average duration of hospital stay was 19.1
±
16.7 days,
with no statistical difference between the A and NA patients
(19.4
±
12 vs 18.8
±
13.8 days, respectively;
p
=
0.79). Total
mortality rate was 17%, with a significant difference between
the A and NA patients (26 vs 10%;
p
=
0.001). The comparison
between A and NA patients is given in Table 2.
Discussion
It has been shown that advanced age is a predictive factor of a
strong prevalence of anaemia in heart failure.
6,8
In our study, the
patients were relatively young, with an average of 57 years, in
comparison with large series in developed countries, where the
median age of patients was 70 years.
9,10
In Africa, very few studies
have been conducted assessing anaemia in HF patients.
11-13
In our study, the prevalence of anaemia in HF was 42%, near
to the 49% that was found in France by Abassade
et al
.,
10
and
lower than the 64.3% found by Kuule
et al
. in Uganda.
11
In the
literature, the prevalence of anaemia is variable, from 4 to 61%,
with the majority of studies finding it between 18 and 20%.
14-16
This large variability may be explained by methodological
differences, due mainly to the definition of anaemia.
2,3,17-19
Most publications use the definition of anaemia by the World
Health Organisation (anaemia is a haemoglobin concentration
<
13 g/dl in men and
<
12 g/dl in postmenopausal women), and
by National Kidney Foundation (anaemia is a haemoglobin
concentration
<
12 g/dl in both men and postmenopausal
women).
20,21
The prevalence of anaemia in our study was therefore
underestimated; it would have been higher if the WHO criteria
for definition had been used.
In chronic HF, factors associated with a high prevalence of
anaemia include concomitant kidney disease, advanced age,
female gender, AfricanAmerican ethnicity, diabetes, hypertension,
and lower estimated glomerular filtration rates.
5,8,22
In our study,
the aetiological research on anaemia was not systematic.
In general, the aetiology of anaemia in chronic HF is
multifactorial, and multiple mechanisms contribute to anaemia
in chronic HF:
15,23
iron and other haematological deficiencies,
renal insufficiency, the role of haemodilution, chronic diseases
and ‘inflammation’, and the renin–angiotensin system. Iron
deficiency appears to be the most common cause of anaemia
in HF.
24,25
In the African context,
26
malnutrition, infectious
pathology (intestinal parasites, HIV infection), and the
congestive nature of HF (salt and water retention, advanced
chronic HF) may partially explain the prevalence of anaemia in
African subjects, the majority being hypertensive and potentially
renal insufficient.
A large number of studies have confirmed that anaemia
is a strong, independent predictor of increased mortality rate
and hospitalisation stay in patients with systolic and diastolic
dysfunction, new-onset HF, and severe chronic HF.
2,4-7,24
In our
study, these reports were confirmed in terms of higher mortality
rate, and longer hospital stay in the anaemic patients compared
to non-anaemic sunjects.
Conclusion
This preliminary study showed a high prevalence of anaemia in
chronic HF patients and its negative impact on the prognosis
(high mortality rate, longer hospitalisation) of patients. The
prognosis of anaemic patients suffering from HF may be
improved by treatment of the anaemia.
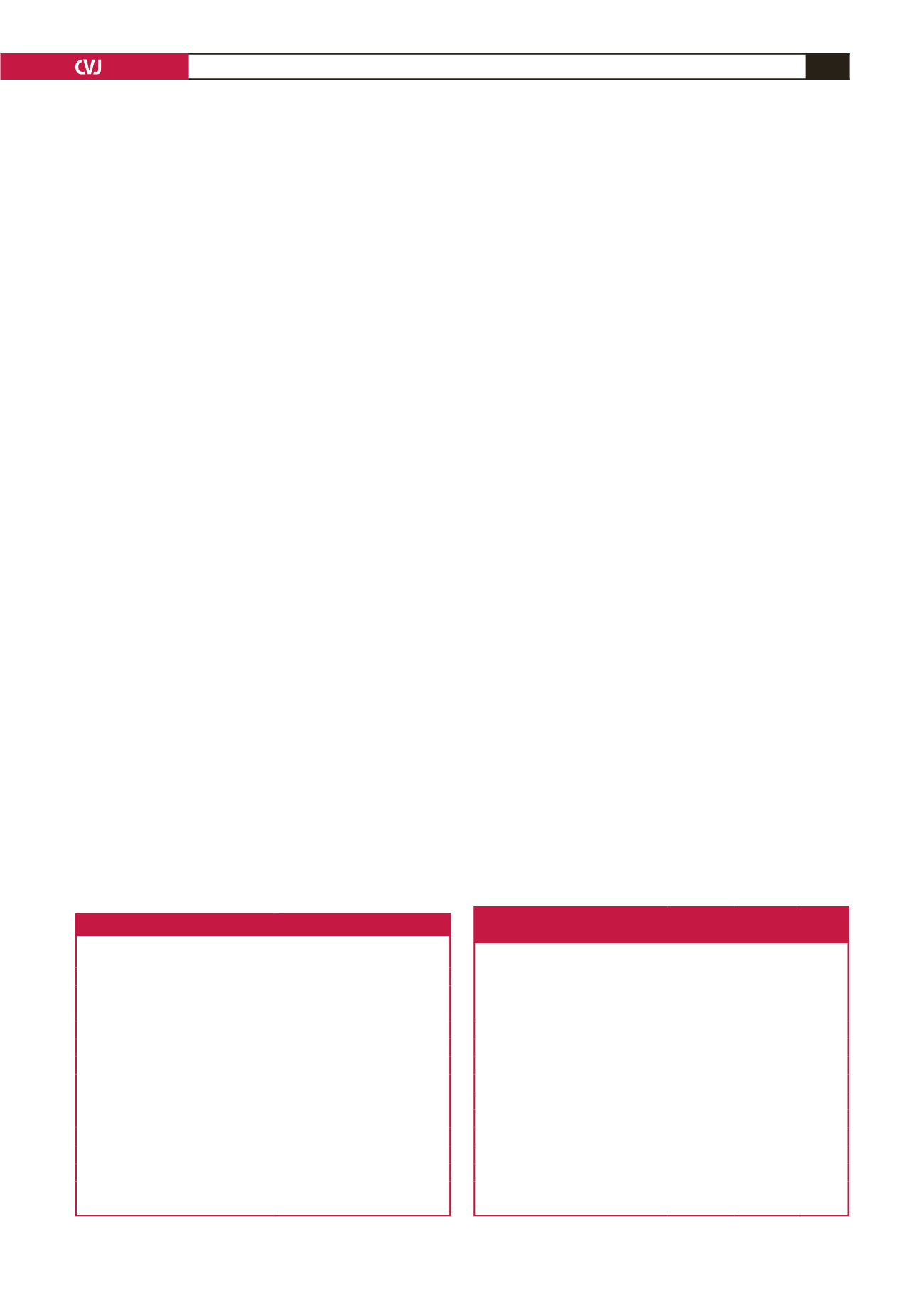
Table 1. Patient characteristics
Parameters
Patients
(
n
=
272)
Male gender,
n
(%)
130 (47.8)
Age (years), SD (range)
56.9
±
16.5 (18–97)
Low socio-economic level,
n
(%)
211 (77.5)
HIV +,
n
(%)
12 (4.4)
Biventricular HF,
n
(%)
233 (85.7)
NYHA III–IV,
n
(%)
249 (91.5)
Haemoglobin (g/dl), SD (range)
11.9
±
4.4 (4.7–15.2)
Aspirin,
n
(%)
15 (5.5)
Oral anticoagulation,
n
(%)
47 (17.3)
LVEF (%), SD (range)
49.3
±
14.7 (22–75)
Hospitalisation stay (days), SD
19.1
±
16.7
Mortality rate,
n
(%)
46 (17)
HIV: human immunodeficiency virus; HF: heart failure; NYHA: New
York Heart Association; LVEF: left ventricular ejection fraction.
Table 2. Comparison between anaemic
and non-anaemic patients
Parameters
Anaemic
patients
(
n
=
114)
Non-
anaemic
patients
(
n
=
158)
p
-value
Age (years)
54.9
±
18.3 58.3
±
15.1 0.105
Haemoglobin (g/dl)
9.4
±
1.8 13.8
±
4.9 0.0001
Biventricular HF,
n
(%)
101 (43.3) 132 (56.7) 0.159
NYHA III–IV,
n
(%)
106 (93)
143 (90.5) 0.6
Aspirin,
n
(%)
3 (2.5)
12 (7.6) 0.06
Oral anticoagulation,
n
(%)
19 (16.7) 28 (17.7) 0.47
LVEF (%)
48
±
14.6 51.3
±
14.9 0.43
Glomerular filtration rate (ml/min) 54.6
±
12.5 70.4
±
10.2 0.004
Hospitalisation stay (days)
19.4
±
12 18.8
±
13.8 0.79
Mortality rate,
n
(%)
30 (26)
16 (10)
0.001
HF: heart failure; NYHA: New York Heart Association; LVEF: left
ventricular ejection fraction.

















