
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 3, May/June 2015
e12
AFRICA
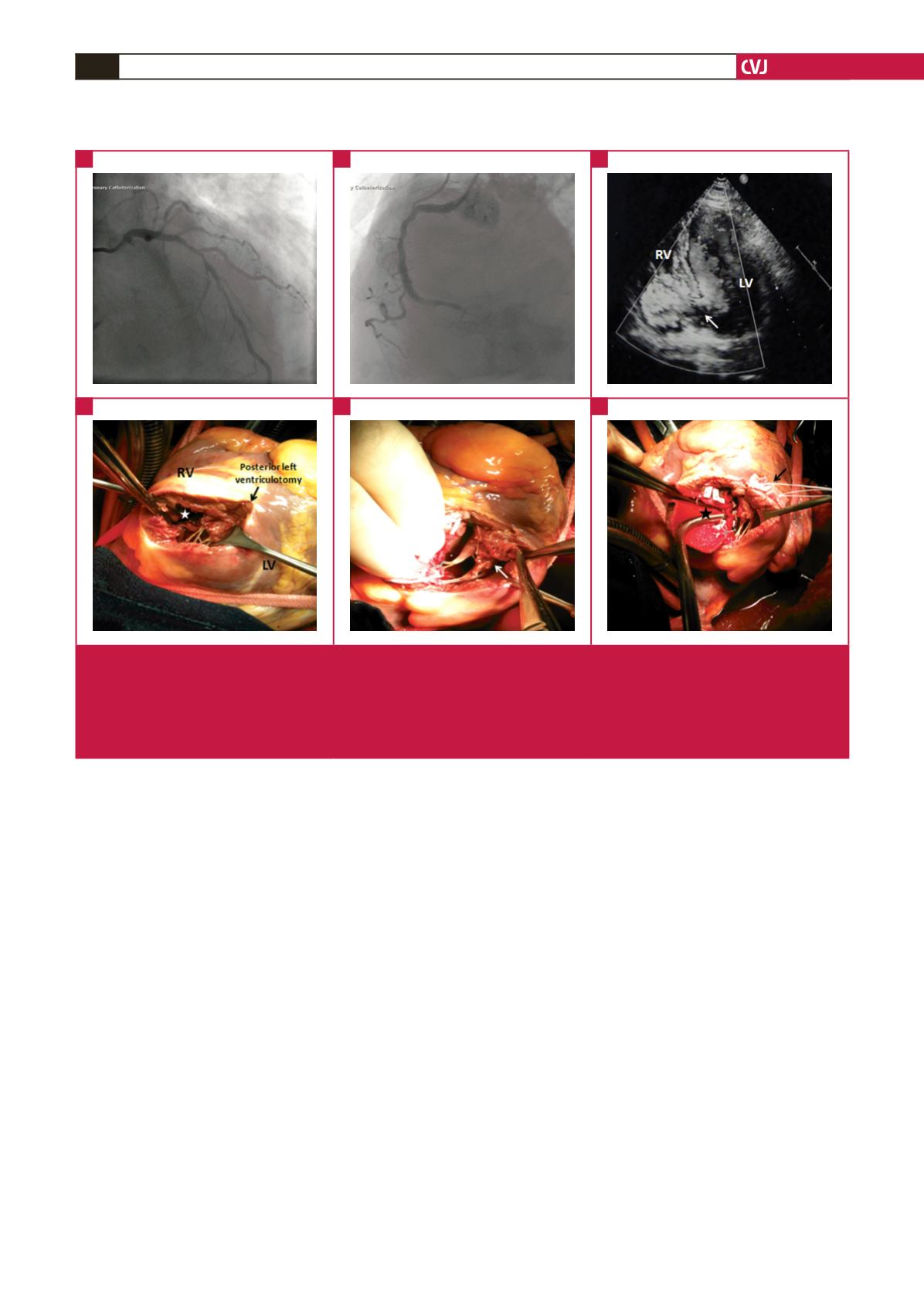
appeared to be necrotic (Fig. 1E). The decayed base of the
posteromedial papillarymusclewas attached to the left ventricular
wall using two interrupted mattress 4-0 polytetrafluoroethylene
(goretex) sutures with a teflon pledget (Fig. 1F). The posterior
left ventriculotomy was closed in two layers over two teflon felt
strips using 2-0 polypropylene sutures (Ethicon, Inc, Somerville,
NJ).
CABG was then performed with sequential grafting of
the saphenous vein to the left anterior descending artery
and second diagonal branch. Peri-operative transoesophageal
echocardiography demonstrated well-preserved left ventricular
wall contraction except for the infarcted area, with no evidence
of residual leak.
Successful weaning from cardiopulmonary bypass was
achieved with an intra-aortic balloon pump (IABP) and low-dose
inotropic support. The patient tolerated the surgical procedure
well, and his initial postoperative course was uneventful. He
remained intubated for 13 hours in ICU with a 24- and 48-hour
postoperative blood loss of 750 and 300 ml, respectively. For 48
hours during the immediate postoperative period, the patient
was managed with intra-aortic balloon counter pulsation and
small doses of inotropic drugs. He was weaned off IABP on the
third postoperative day.
A total dose of 98 500 IU of heparin was given before (72 000
IU) and during (26 500 IU) cardiopulmonary bypass (CPB) at
our hospital. Anticoagulation was reversed by protamine at the
end of the operation. Following separation from bypass, the
patient was given a total of six units of fresh frozen plasma and
eight units of packed red cells.
Blood tests were done regularly and the platelet count was
monitored daily. Laboratory findings on admission showed a
normal platelet count (210
×
10
3
cells/
μ
l). Thrombocytopaenia
developed postoperatively on day four with falls in platelet count
of more than 50%, with a platelet level of 64
×
10
3
cells/
μ
l, from
an initial admission count of 210
×
10
3
cells/
μ
l. The nadir platelet
count was 25
×
10
3
cells/
μ
l on the seventh postoperative day (Fig.
2). Fig. 2 summarises the patient’s platelet counts and key clinical
events during hospitalisation.
On postoperative day five, right-hand cyanosis was noted with
absent radial pulses and was attributed to the presence of a right
radial arterial catheter. The radial arterial catheter was removed
the same day without improvement. Doppler ultrasound showed
an occlusion of the radial artey and a patent ulnar artery. Also,
a superficial venous thrombosis (cephalic and basilic vein) was
detected in the right arm by Doppler ultrasound.
On postoperative day six, ischaemic changes developed on
the front of both feet (Fig. 3). The ischaemic changes in the
right hand worsened from that of the previous day. Additionally,
an occlusion of the right ulnar artery was detected by Doppler
ultrasound. A brachial artery thrombectomy was performed
Fig. 1.
(A, B) Coronary angiography showing critical stenoses of the left anterior descending artery and ostium of the second diago-
nal branch, and occlusion of the right coronary artery. (C) Transthoracic echocardiography showing post-infarction postero-inferior
ventricular septal rupture (VSR) (white arrow). (D) Surgery photograph showing VSR (white asterisk) and (E) necrotic and decayed
basal portion of the postero-medial papillary muscle (white arrow). (F) Surgery photograph showing that the VSR was closed (black
asterisk) with a patch and the posteromedial papillary muscle was attached to the left ventricular wall with polytetrafluoroethylene
sutures (black arrow). LV: left ventricle, RV: right ventricle.
A
D
B
E
C
F

















