
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 6, November/December 2015
AFRICA
235
even necrosis.
7
Myocardial ischaemia causes intracellular calcium
accumulation and degradation of the membrane lipids, and
oedema during ACC. After removal of the aortic cross-clamp,
reperfusion causes oxidative stress depending on the production
of reactive oxygen (ROS) and reactive nitrogen species (RNS).
8
In addition, it has been reported that myocardial ischaemia–
reperfusion (I/R) induces cardiomyocytic apoptosis.
9,10
Early and accurate detection of PMI may prompt immediate
improvement in the perfusion and oxygen demand of the
myocardium,which may limit PMI. Therefore, it is important to
have a highly specific diagnostic marker to detect PMI.
Cardiac surgery may lead to the release of markers of
myocardial injury. Interpretation of these elevated cardiac
markers in the blood during the peri-operative period is
confusing because increases in cardiac markers may be related
to direct skeletal muscle injury due to the surgical procedure, or
to myocardial I/R injury. It is diffucult to differantiate between
increases in cardiac markers related to surgical procedure and
pathological myocardial I/R injury.
11
In this study, we considered that histopathological
examination of myocardial tissue would clearly reveal myocyte
damage occurring in the peri-operative period, and increases in
cardiac markers could be properly interpreted, comparing them
with the results of the histopathological examination. To the best
of our knowledge, the relationship between severity of PMI and
apoptosis, and the cardiac markers assayed in this study has not
been previously studied in CABG surgery with CPB.
This study therefore had the following objectives: (1) to
examine whether PMI, as occurs during CABG surgery, is
associated with myocardial apoptosis and the release of cardiac
markers, using biochemical and histopathological analysis; (2)
to determine whether there is a direct relationship between the
release of cardiac markers and the severity of myocardial injury
and apoptosis, as graded histopathologically; and (3) to compare
efficacies of cardiac markers to detect PMI rapidly and accurately.
Methods
This prospective study was carried out in Dumlupinar University
Evliya Celebi Research and Education Hospital, Turkey, between
April and September 2014. The study was in accordance with
the principles outlined in the Declaration of Helsinki. Ethical
approval was received from the local Human Research Ethics
Committee (no: 2013/14-122). Written informed consent was
obtained from the all patients.
The study population consisted of 37 patients (24 male, 13
female, mean age 63.4
±
8.9 years) undergoing elective CABG
who fulfilled the inclusion criteria. Inclusion criteria were age
over 18 and less than 80 years, and need for elective myocardial
revascularisation for angina pectoris. The exclusion criteria
included ejection fraction
<
30%; recent anterior myocardial
infarction (
<
one month), the requirement of a concomitant
cardiac operation, emergency surgery or re-operation.
Demographic, pre-operative and intra-operative data of patients
are shown in Table 1.
Anesthesia, CPB and surgical procedure
The same surgical and anesthetic team managed all patients.
Cardiopulmonary bypass and surgical techniques were
standardised and did not change during the study period.
Pre-medication, general anaesthesia with endotracheal
intubation, and transfusions were the same in all cases. Induction
of anaesthesia was performed using 5–10 mcg/kg fentanyl,
3–5 mcg/kg thiopental, 0.05 mg/kg midazolam and 0.1 mg/kg
vecuronium. Anaesthesia was maintained using 2% sevoflurane
and 1–3 mcg/kg/dk remifentanil.
A median sternotomy was performed with a midsternal
incision, followed by routine aortic and right atrial cannulation.
After harvesting the bypass graft conduits (left internal mammary
artery and saphenous vein) the patients were prepared for CPB.
Anticoagulation was achieved with 400 U/kg heparin. CPB was
carried out using membrane oxygenators and moderate systemic
hypothermia.
Myocardial protection was achieved with combined antegrade
and retrograde continuous mild hypothermic (32°C) blood
cardioplegia. The contents of the cardioplegia solution were as
follows: 80 mEq potassium, 12 mEq magnesium and 44 mEq
sodium bicarbonate in 0.9% saline, and this solution was diluted
with blood in a ratio of 1:4.
Aortic cross-clamping was performed and diastolic arrest
was achieved by cardioplegia. After the distal anastomoses were
completed, the aortic cross-clamp was removed and the proximal
anastomoses were performed on the aorta during myocardial
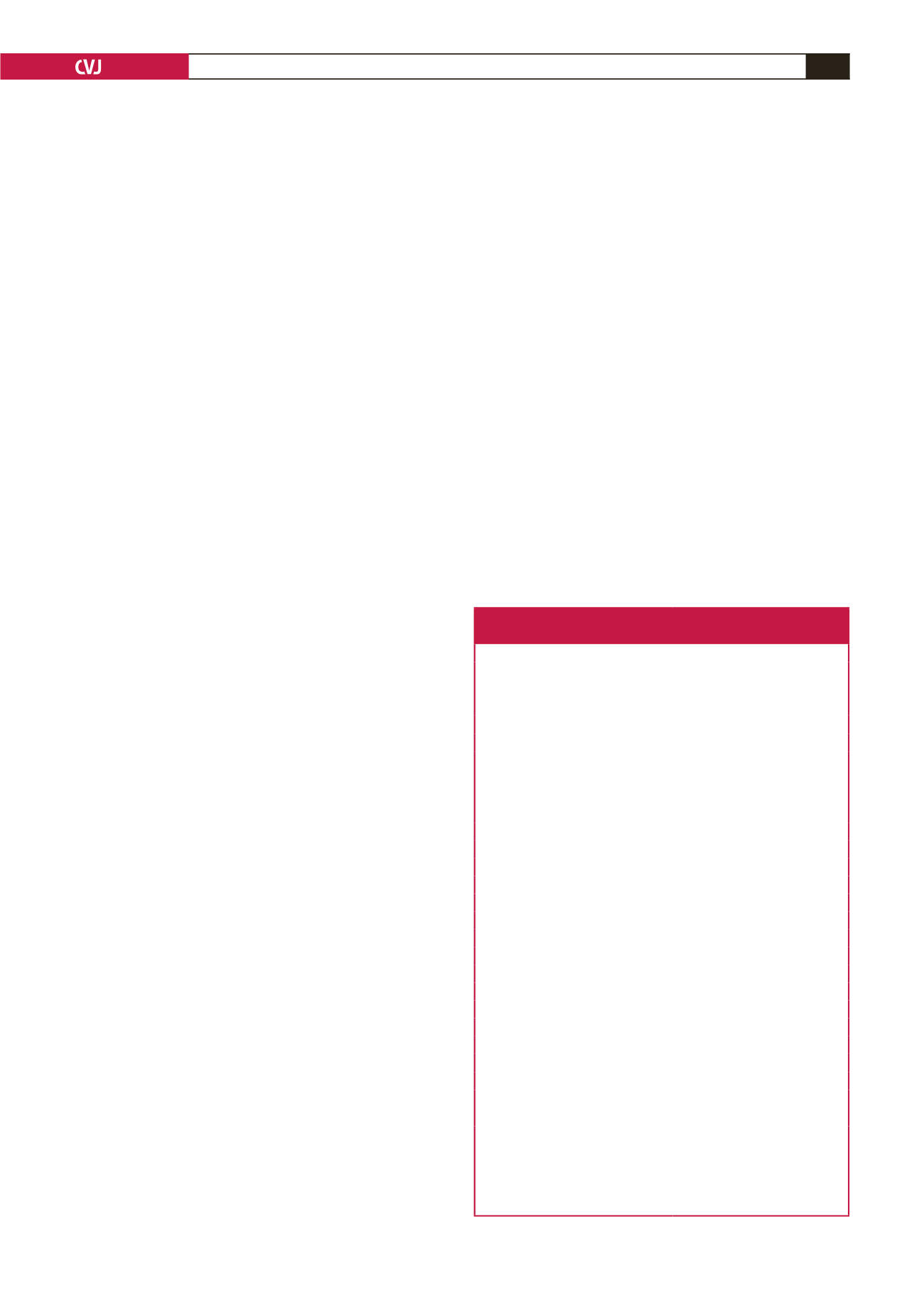
Table 1. Demographic, pre-operative and
intra-operative data of the patients
Parameters
n
=
37
Age (years)
63.4
±
8.9
Male (
n
)
24
Female (
n
)
13
Weight (kg)
75.8
±
13.7
Height (cm)
162.7
±
8.6
BMI (kg/m
2
)
28.67
±
4.8
NYHA classification (
n
)
Class I
21
Class II
14
Class III
2
LVEF (%)
Normal (> 50%)
23
Moderate (31–49%)
14
MI history (
n
)
15
Medication (
n
)
β
-Blockers
33
ACE inhibitors
8
Calcium antagonists
11
Statins
30
Acetylsalicylic acid
35
Other anticoagulants
4
ACC time (min)
56.7
±
15.3
CPB time (min)
101.9
±
23.4
Grafted vessels (
n
)
3.17
±
0.62
Apoptotic index (TUNEL, %)
25.7
±
8.4
Myocardial injury score
1.5
±
0.5
BMI: body mass index; NYHA: New York Heart Association; LVEF:
left ventricular ejection fraction; MI: myocardial infarction; ACE:
angiotensin converting enzyme; ACC: aortic cross-clamping; CPB:
cardiopulmonary bypass; TUNEL: terminal deoxynucleotidyl trans-
ferase-mediated deoxyuridine triphosphate nick end-labelling; SD:
standard deviation. Data are presented as median
±
SD or number.

















