
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 3, May/June 2016
156
AFRICA
Cox’s proportional hazards regression showed that survival
was predicted by NYHA functional class at last visit (
p
=
0.026),
but not by presence of a disease-causing mutation (
p
=
0.474),
as shown in Figs 1B and 1C, respectively. Survival in this cohort
was similar to that of an age- and gender-matched general South
African population (Fig. 1D).
The presence of chronic heart failure [hazard ratio (HR)
4.4, 95% CI: 1.0–18.3;
p
=
0.044] and NYHA functional class
at last visit (HR: 6.2, 95% CI: 1.2–30.6;
p
=
0.026) were found
to be predictors of mortality on univariate regression analysis.
On multivariate analysis, both chronic heart failure and NYHA
functional class were not significant as predictors of mortality,
as they may be proxies for LVEF (Table 6).
Discussion
To our knowledge this is the first prospective study of the
clinical profile, spectrum of disease-causing gene mutations and
outcome in HCM from the African continent, including black
Africans. Age at onset of symptoms (38.5
±
14.3 years), male
preponderance (58%), and major symptoms were similar to
those reported in North American, Middle Eastern and Eastern
series (Table 2).
11,16,17
Nearly 30% of the patients bear mutations
in the
MYH7
and
MYBPC3
genes, which are the commonest
genetic causes of HCM.
15
While the annual mortality rate of 2.9% was high and the
overall survival of 74% at 10 years was low compared to other
series of patients with HCM,
11
the survival rate was comparable
to age- and gender-matched members of the South African
population. Survival was predicted by NYHA functional class
at last visit.
We have found that HCM occurs predominantly in men,
with a young age of onset, including black Africans, and with
a positive family history of HCM in the majority. Fatigue,
breathlessness and palpitations were the commonest symptoms.
Atrial fibrillation was found in 9%, left ventricular outflow tract
obstruction in 28%, and diastolic dysfunction in most.
In a study of the natural history of HCM in non-hospitalised
Americans, Maron and others found that 55% of patients were
men, the mean age was 47 years, and cardiac symptoms were
present in 63% of patients.
11
Similarly, in a study from Taiwan,
Lee and colleagues found 52% HCM patients to be male,
and that men had a younger age of onset of HCM compared
to women.
16
In this study, the prevalence of apical HCM
was three times higher in men, and interestingly, men had a
lower prevalence of LVOT obstruction. Thirty-six per cent of
Taiwanese HCM patients had pulmonary oedema or paroxysmal
atrial fibrillation. More recently, in the first report on the clinical
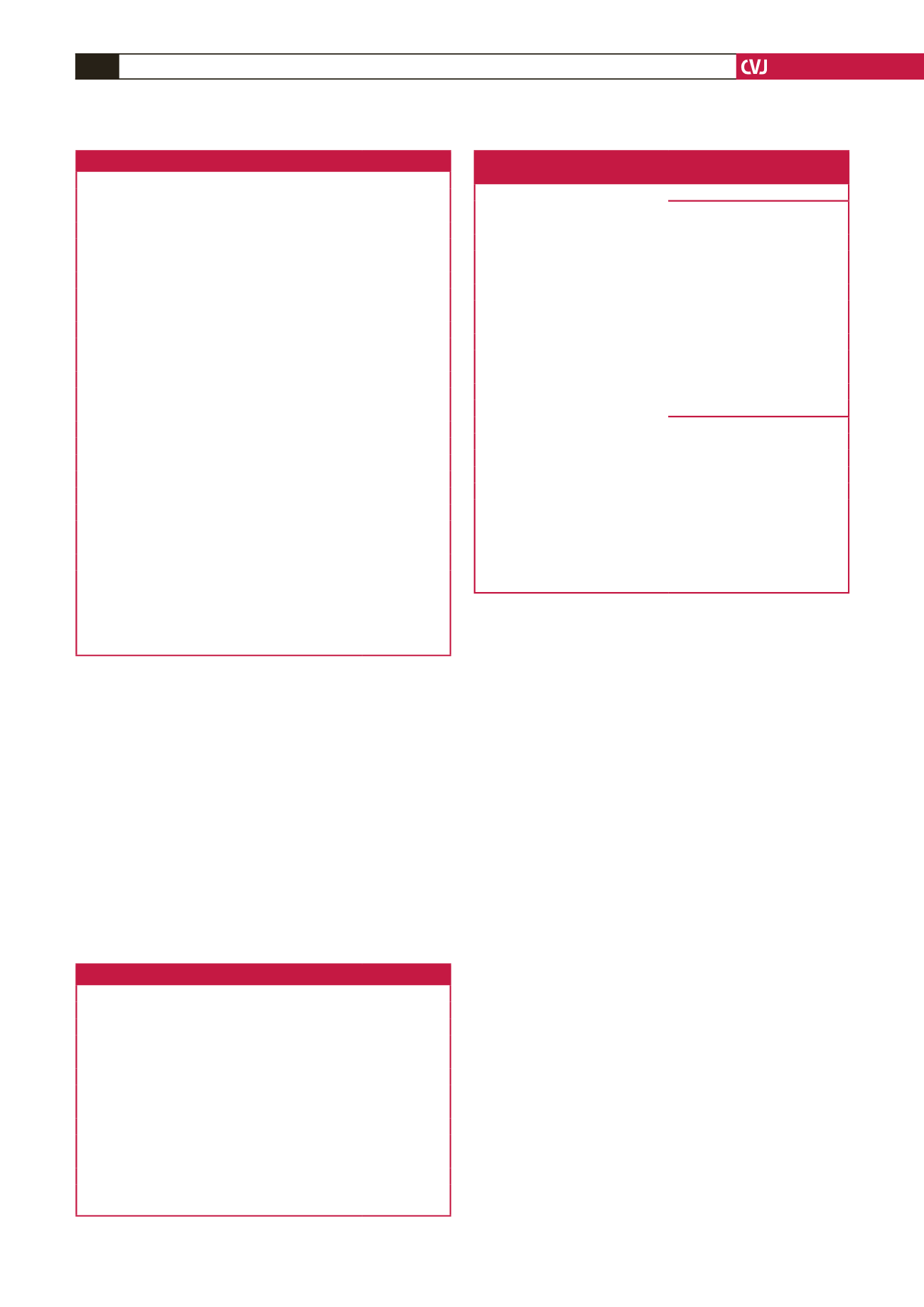
Table 4. Follow-up and outcome data
Outcome data
n
(%)
Mean duration of follow up (years
±
SD)
9.1
±
3.4
Total number of mutations per person
12.8 (3.2)
Follow-up observation
Regular
37 (86.0)
Lost to follow up
6 (14.0)
Death
8 (18.6)
Chronic heart failure
11 (25.6)
ICD insertion
0 (0)
PPM insertion
0 (0)
CRT/biventricular pacing
0 (0)
Loop recorder
6 (14.0)
Arrhythmia present
No arrhythmia
32 (74.4)
Atrial fibrillation
8 (18.6)
Atrial flutter
1 (2.3)
Ventricular tachycardia
2 (4.7)
Myomectomy
3 (7.0)
Alcohol septal ablation
1 (2.3)
Evolution to DCM
4 (9.3)
Orthotopic heart transplantation
1 (2.3)
NYHA functional class at last visit
I and II
31 (72.1)
III and IV
12 (27.9)
Stroke
4 (9.3)
All values are number (percentage), unless otherwise stated.
ICD, implantable cardioverter defibrillator; PPM, permanent pacemaker; CRT,
cardiac resynchronisation therapy; DCM, dilated cardiomyopathy; NYHA,
New York Heart Association functional classification for evaluation of severity
of dyspnoea.
Table 5. Medical therapy at follow up
Therapy
n
(%)
β
-blocker
33 (76.7)
Calcium channel blocker
17 (39.5)
Warfarin
12 (27.9)
ACEI or ARB
9 (20.9)
Furosemide
8 (18.6)
Aspirin
8 (18.6)
Disopyramide
4 (9.3)
Spironolactone
4 (9.3)
Amiodarone
3 (7.0)
Digoxin
2 (4.7)
Nitrates
1 (2.3)
ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor
blocker;
β
-blocker, beta-blocker.
Table 6. Cox’s proportional hazards regression model analysis of
predictors of mortality in hypertrophic cardiomyopathy
Univariate Cox regression
Variables
Hazard ratio (95% CI)
p
-value
Age at diagnosis
1.0 (1.0–1.1)
0.561
Mutation positive
1.8 (0.4–8.9)
0.474
Sarcomeric mutations
1.3 (0.5–3.5)
0.585
Total number of mutations per person
1.12 (0.91–1.3)
0.412
IVS
1.6 (0.8–3.4)
0.169
LVEF
1.1 (1.0–1.2)
0.060
Family history of SCD
0.8 (0.1–6.6)
0.840
E/A ratio
2.0 (0.4–10.0)
0.370
Loop recorder
3.5 (0.8–14.6)
0.088
Chronic heart failure
4.4 (1.0–18.3)
0.044
NYHA functional class at last visit
6.2 (1.2–30.6)
0.026
Multivariate Cox regression
Variables
Hazard ratio (95% CI)
p
-value
LVEF
1.1 (1.0–1.2)
0.100
Loop recorder
0.8 (0.1–5.3)
0.828
Chronic heart failure
1.6 (0.2–16.2)
0.684
NYHA functional class at last visit
4.2 (0.4–41.3)
0.218
E/A, ratio of early (E) to late (A) ventricular filling velocities on Doppler
echocardiography; IVS, interventricular septal thickness in diastole; HCM,
hypertrophic cardiomyopathy; LVEF, left ventricular ejection fraction; NYHA,
New York Heart Association functional classification for severity of breathless-
ness; SCD, sudden cardiac death. In the univariate and multivariate regression
analysis, NYHA was correlated as a binary variable (NYHA FC I–II vs NYHA
FC III–IV).

















