
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 1, January/February 2017
6
AFRICA
However, the groups did not differ significantly with regard to
gender; BMI; prevalence of diabetes mellitus, hypertension and
hyperlipidaemia; and smoking status.
The echocardiographic parameters of the groups are presented
in Table 2. The MPI was higher in the high-GS group of patients
than in the low- and mid-GS groups (
p
<
0.001). IVRT was
significantly higher in the high-GS group than in the other
groups, and the difference was significant between the high- and
low-GS groups, and between the high- and mid-GS groups (
p
=
0.005). Furthermore, ET was significantly lower in the high-GS
group (
p
<
0.001), whereas the EF was similar in the low- and
mid-GS groups, although the high-GS group had a significantly
lower EF (
p
=
0.01).
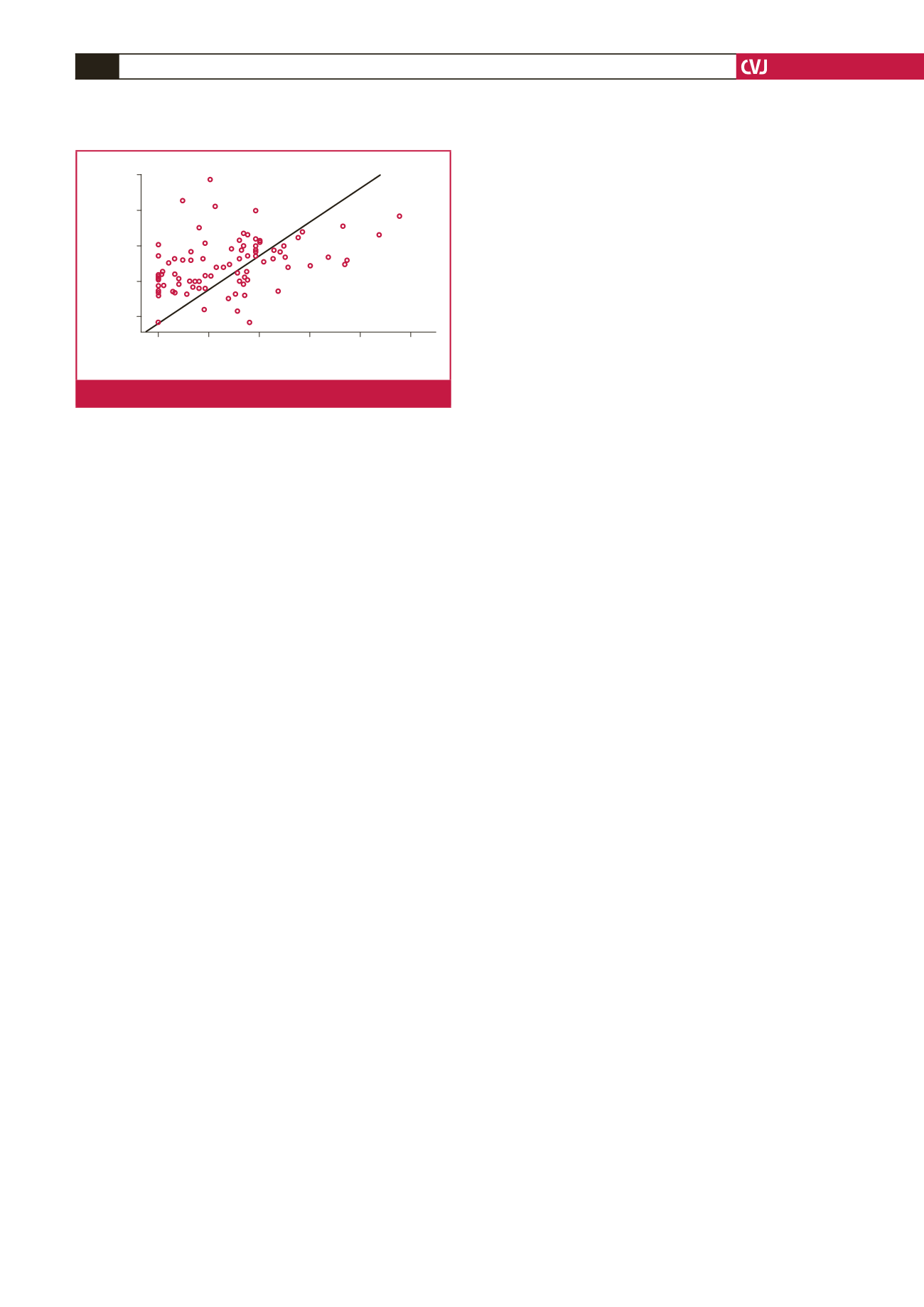
Correlation analysis was performed to investigate the
relationship between the MPI, age and GS. MPI was positively
correlated with GS (
r
=
0.47, p
<
0.001; Fig. 1), and age and GS
showed a weak positive correlation (
r
=
0.25,
p
=
0.01).
Multivariate regression analysis for predictors of GS included
age and MPI. MPI was identified as an independent predictor of
GS (
β =
0.358,
p
<
0.001).
Discussion
In this study, we found that the risk of significant lesion
complexity increased progressively with increasing MPI.
According to our results, MPI is an independent predictor of
GS, a measure of the severity of coronary artery disease.
Assessment of systolic and diastolic function by non-invasive
methods in patients with AMI is of great importance for risk
stratification and prognosis.
5
EF, as determined by routine
2D echocardiography, is the most widely used instrumental
parameter for the evaluation of left ventricular function, but
this parameter focuses only on systolic function. Both systolic
and diastolic functions are frequently affected during an AMI,
and therefore, a combined measurement of left ventricular
performance may be more useful in assessing overall cardiac
function than systolic or diastolic measures alone.
MPI, also known as the Tei index, reflects both systolic and
diastolic function of the left ventricle. MPI is calculated using
the following formula: (IVCT
+
IVRT)∕ET.
4
During the acute
phase of an AMI, IVCT and IVRT increase, and when clinical
heart failure becomes apparent, the ET decreases. As a result,
MPI increases.
6
MPI is rapidly increased in the early phase of MI and
the degree of increment is associated with both mortality
and morbidity.
7
Several studies show that MPI tends to be
significantly higher in patients with AMI,
8,9
but these studies
do not describe the type of AMI or the severity of coronary
involvement.
Sahin
et al
.
10
showed that MPI changed in proportion to
the severity of CAD in patients with stable CAD, who had
an increased prevalence of risk factors such as diabetes and
hypertension. However, the increased MPI in that study may
have been related to these risk factors, because MPI is reported
to be impaired in patients with diabetes and hypertension.
11
To the best of our knowledge, our study is the first to
demonstrate the relationship between MPI and GS in patients
with NSTEMI. In this study, the prevalence of risk factors did
not differ among groups of patients classified according to the
GS, and MPI was an independent predictor of GS.
There are two treatment strategies for patients with NSTEMI:
invasive and conservative. Determination of the number of
diseased coronary arteries is important in the decision-making
process when selecting the course of treatment. The severity
of coronary artery disease is associated with mortality in
patients with acute coronary syndromes.
12
In the early period of
NSTEMI, measurement of MPI may be useful in the decision-
making process, for selecting the course of treatment and risk
stratification.
Our study has some limitations. First, assessment of coronary
angiographic findings was limited to visual interpretation, with
inter- and intra-observer variability. Second, the sample size was
small and no calculations were made to ensure that the study was
adequately powered.
Conclusion
MPI was an independent predictor of GS in patients with
NSTEMI. Patients with NSTEMI who are at high risk may be
identified by a simple MPI measurement, which can be useful
in the decision-making process for treatment selection and risk
stratification.
References
1.
Gensini GG. More meaningful scoring system for detemining the sever-
ity of coronary artery disease.
Am J Cardiol
1983;
51
(3): 606. PubMed
PMID: 6823874.
2.
Peppes V, Rammos G, Manios E, Koroboki E, Rokas S, Zakopoulos
N. Correlation between myocardial enzyme serum levels and markers
of inflammation with severity of coronary artery disease and Gensini
score: A hospital-based, prospective study in Greek patients.
Clin Interv
Aging
2008;
3
: 699–710. PubMed PMID: 19281062.
3.
Zhenhong F, Yundai C, Wei D, Lian C, Luyue G, Hongbin L,
et al
.
Correlation between coronary artery lesion severıty and long-term
clinical outcomes in Chinese Han octogenarians with acute coronary
syndrome.
Heart
2012;
98
: E191.
4.
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ,
et al
.
New index of combined systolic and diastolic myocardial performance:
a simple and reproducible measure of cardiac function – a study in
normal and dilated cardiomyopathy.
J Cardiol
1995;
26
: 357–366.
PubMed PMID: 8558414.
5.
Moller JE, Egstrup K, Kober L, Poulsen SH, Nyvad O, Torp-Pedersen
C. Prognostic importance of systolic and diastolic function after acute
Gensini score
0
50
100
150
200
250
Myocardial performance index
1.25
1.00
0.75
0.50
0.25
r
=
0.47
p
<
0.001
Fig. 1.
Correlation between MPI and Gensini score.

















