
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 1, January/February 2017
10
AFRICA
within the first three months of delivery, and two (4.7%) between
four and five months postpartum.
On enrolment, all the patients were already on some form
of treatment for heart failure; 38 (88.4%) were on diuretics,
28 (65.1%) were on angiotensin converting enzyme inhibitors
(ACEIs) or angiotensin receptor blockers (ARBs) and 26
(60.5%) were on spironolactone. In comparison, only eight
(18.6%) patients were on beta-blockers (two on atenolol, six on
carvedilol). The mean ejection fraction of the cohort at baseline
was 29.7
±
9.8% and four (9.3%) patients had left ventricular
thrombi.
Table 2 shows the change in NYHA functional class between
the three points. There was a significant improvement in NYHA
from baseline to each of the time endpoints (
p
<
0.001 for both).
By three months, 20 (54.1%) patients were in NYHA class I
and only two (5.4%) were in NYHA IV. Of the two patients
in NYHA IV, one had completely defaulted on treatment and
the other had been on suboptimal therapy. By six months, 23
(65.7%) patients had an NYHA class of I compared to only one
patient with an NYHA class of IV.
Table 3 summarises the changes in left ventricular function.
Patients who completed six months of treatment showed a
significant improvement in the ejection fraction from 29.7
±
9.8% at baseline to 44.9
±
14.9% after six months (
p
<
0.001).
Increases in LVEF between all time points were statistically
significant, except for those that occurred between baseline and
three months (
p
<
0.05).
There was a non-significant reduction in LVDd from 56.8
±
6.6 mm at baseline to 53.4
±
9.2 mm after six months. By
three months after diagnosis eight (22.3%) of the patients had
a normal LVEF and eight (22.3%) showed remarkable LVEF
improvement. Of the 35 patients who completed six months of
follow up, 15 (42.9%) had normalised left ventricular function.
Remarkable improvement of LVEF was seen in 16 (45.7%)
patients after six months of follow up.
Of the five (11.6%) patients who died during the study period,
four (9.3%) died within the first three months of diagnosis.
Two (40.0%) died from progression of heart failure while still
hospitalised. Of the three who died outside the hospital, one died
of thromboembolic disease, based on a post mortem that showed
right leg deep venous thrombosis, a left ventricular thrombus
and a large pulmonary embolus. There was no reported cause of
death for the other two patients, although one had an intramural
thrombus on echocardiography at three months and the other
had presumed upper limb deep venous thrombosis, based on
clinical examination.
Discussion
PPCM has never been studied before in Zimbabwe. This study
looked at the natural history of this rare condition in a relatively
large cohort of Zimbabwean patients with a mean age of 27.9
±
6.0 years. The majority of the women were primigravidas and
a large proportion had been diagnosed with pregnancy-induced
hypertension, however none of them were hypertensive at diagnosis.
The LVEF had normalised in a large proportion (42.9%)
of the patients and the NYHA functional class had improved
significantly after six months of follow up. Still, mortality
was relatively high (11.6%), with progressive heart failure and
thromboembolic disease being the main causes of death.
Demakis, in his landmark study on PPCM, noted that the
condition was ‘more common in the older multiparous woman
and in women who have had toxemia and twins’.
5
Patients who
develop PPCM in Zimbabwe have a clinical profile similar to
those described in previously published reports, with a few
Table 2. NYHA class at baseline, and three and six months
Parameters
Baseline
(n = 43),
n
(%)
3 months
(
n
= 37),
n
(%)
6 months
(
n
= 35),
n
(%)
p
-value
NYHA class
<
0.001**
I
0
20 (54.1)
23 (65.7)
II
23 (53.5)
13 (35.1)
9 (25.7)
III
13 (20.2)
2 (5.4)
2 (5.7)
IV
7 (39.5)
2 (5.4)
1 (2.9)
**Significant at
α
= 1%
Table 3. Left ventricular systolic function at baseline, and three and six months
Baseline
3 months
6 months
0–3 months
p
-value
0–6 months
p
-value
3–6 months
p
-value
All
p
-value
LVDd (mm)
56.8
±
6.6
53.9
±
8.2
53.9
±
9.2
0.345
0.204
1
0.136
LVEF (%)
29.7
±
9.8
36.8
±
13.7
44.9
±
14.9
0.05
<
0.001**
0.028
<
0.001**
*Significant at
α
= 5%, **significant at
α
= 1%.
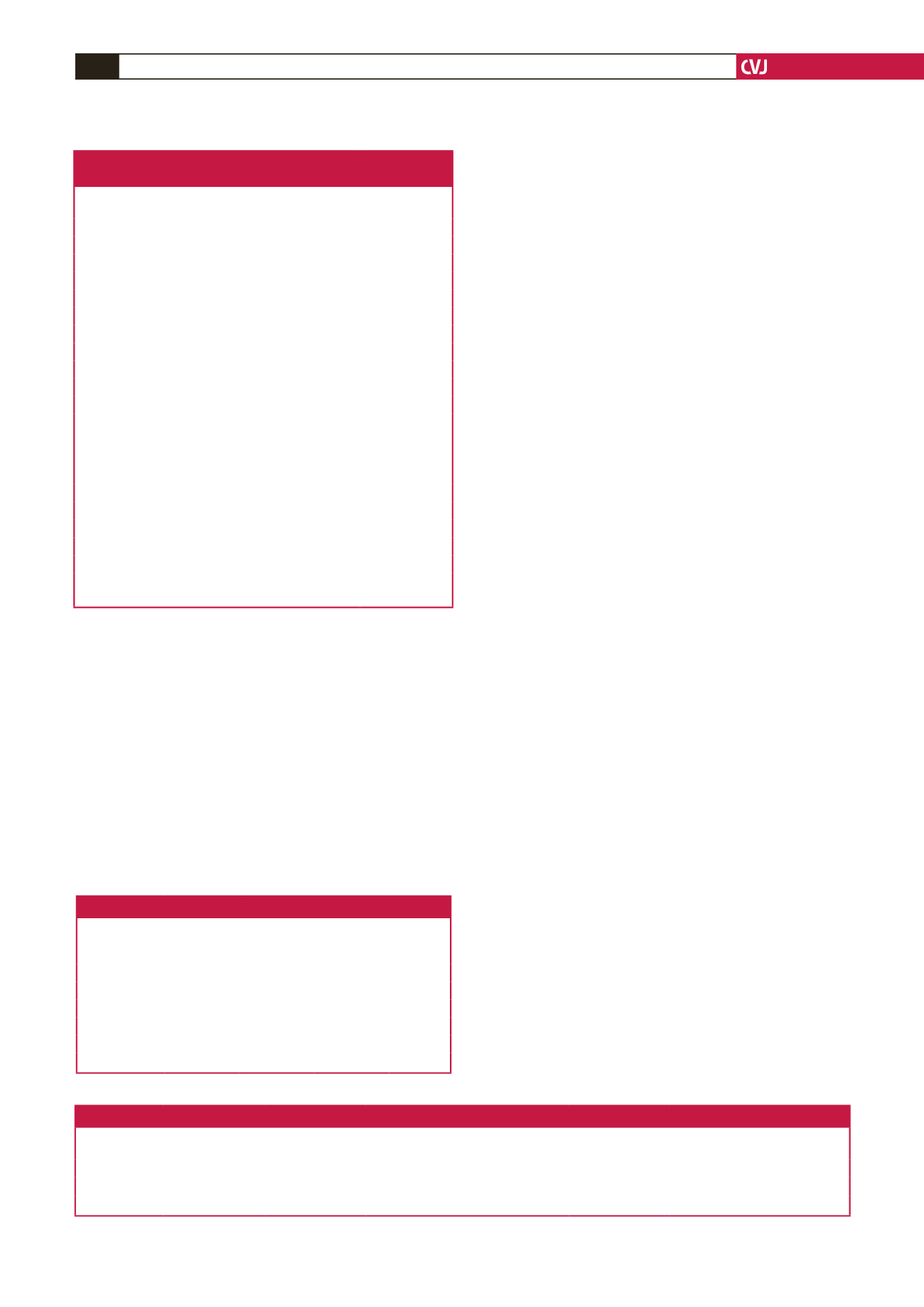
Table 1. Baseline demographic and clinical
characteristics of study patients
Variable
Frequency,
n
(%)
Age (years)
27.9 (6)
Parity
1
15 (34.9)
≥
2
28 (65.1)
NYHA functional class
II
23 (53.5)
III
13 (30.2)
IV
7 (16.3)
Pregnancy-induced hypertension
15 (34.9)
Gestation type
Singleton
40 (93.0)
Twins
3 (7.0)
Time of symptom onset
Pre-partum
1 (2.3)
1–3 months post-partum
40 (9.3)
4–5 months post-partum
2 (4.7)
Echocardiographic data
Left ventricular end-diastolic diameter (mm, range) 56.8 (43.2–72.2)
Ejection fraction (%, range)
29.7 (4.4–50)*
Left ventricular thrombus
4 (9.3)
*A single patient had an LVEF
>
45% but fractional shortening was
<
30%.

















