
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 2, March/April 2017
96
AFRICA
of BMI (
p
<
0.05), WHtR and WC. There was no significant
difference between the AUC of BMI and that of WHtR and WC.
The predictive powers of the four indices were higher in male
than female participants.
For prehypertension, BMI, WC, PI and WHtR had higher
predictive potentials for both genders, with BMI showing slightly
higher power among the four indices. BMI and PI seemed to
perform better in virtually all age groups than the other two
indices.
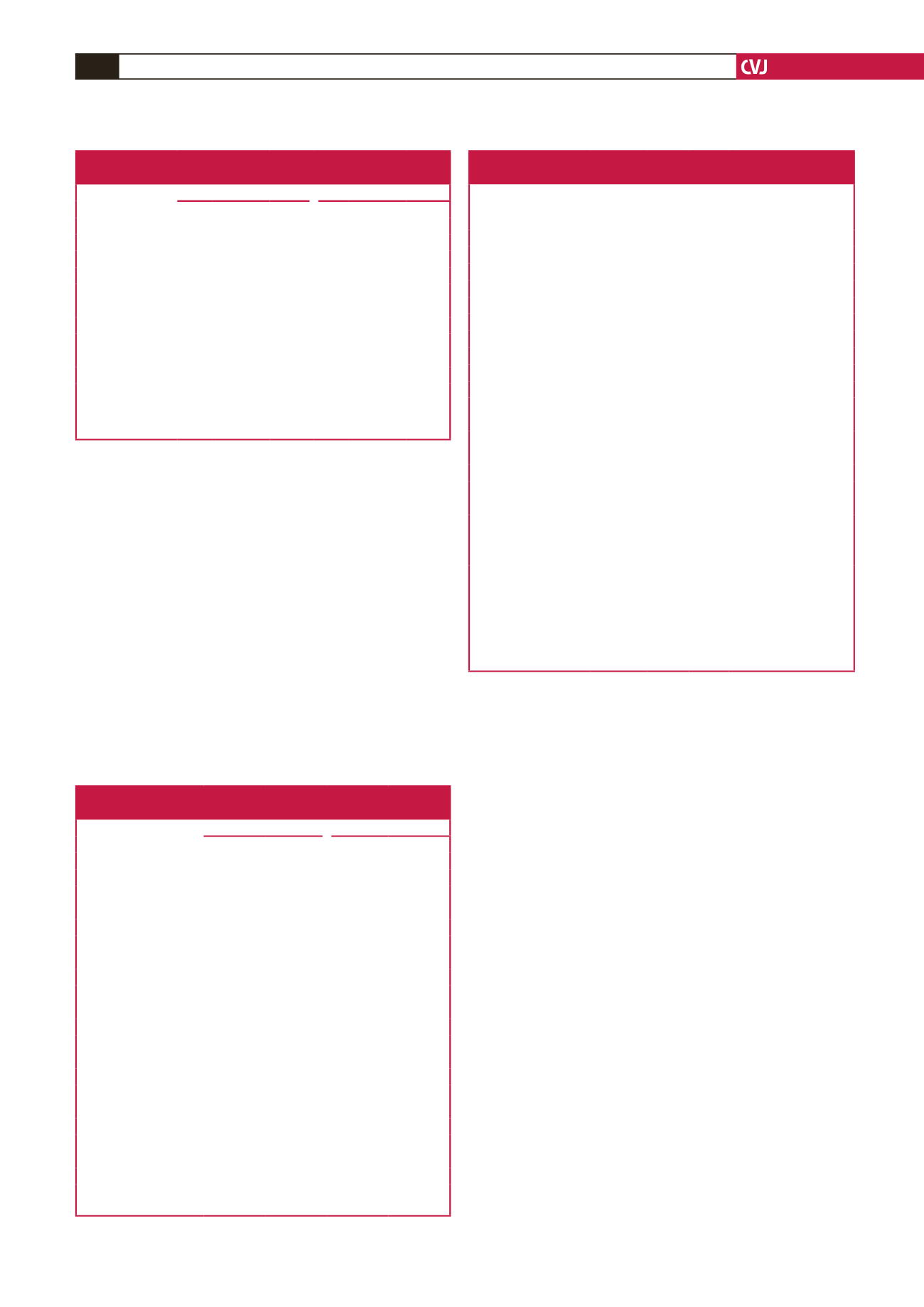
Table 5 examined the possible linear relationship between
the four best anthropometric indices and hypertension and
prehypertension prevalence (risk). The anthropometric indices
were considered as continuous variables to calculate prevalence
ratios corresponding to one standard deviation change. The
hypertension prevalence ratio increased by 15% (WHtR),
15% (WC), 14% (BMI) and 12% (PI) with one standard
deviation increase in the corresponding anthropometric index on
adjusting for gender, age, alcohol intake and physical activity; the
prehypertension prevalence ratio increased by 4% (WHtR), 11%
(WC),11% (BMI) and 6.7% (PI).
Table 6 lists the cut-off points and Youden index J for the
four best anthropometric indices in predicting hypertension and
prehypertension. The best Youden index J was recorded in BMI
and WHtR for all categories but this was not strikingly distinct.
The effect of other anthropometric indices on BMI prevalence
ratio, as well as its hypertension predictive power is shown in
Table 7. On average, each unit increase in BMI was associated
with a 26 and 14% increase in prevalence ratio for hypertension
in the male and female categories, respectively (model 1
p
>
0.05 in most cases). There was about a 17 and 4% increase in
prevalence ratio associated with one unit increase in BMI in
model 2 in males (
p
<
0.05) and females (
p
>
0.05), respectively.
The combination of WC, WHtR and PI did not change
the prevalence ratio beyond 10%, except for PI, which gave
percentage changes of 13.58 and 9.87% for model 1 and 2,
respectively in males. The changes due to the addition of WC
and WHtR were generally decremental, while that of PI was
incremental. On average, the changes in PR were higher in
model 1 compared to model 2. There was an increase in model
fit (AUC) when WC, WHtR or PI were used in model 1 and 2,
except for PI in model 1, which resulted in a slight decrease in
AUC when compared with BMI only. However, none of the
percentage changes in the AUCs of each model was
<
2% (
p
<
0.05 in almost all models for males and
>
0.05 in all models for
females.)
Table 7. Gender-specific prevalence ratios and
AUCs of BMI for hypertension
Male
PR 95% CI
p
-value
% PR
change AUC
% AUC
change
p
-value
Model 1
BMI
1.10 1.07–1.14 0.000 – 0.6978 –
BMI
+
WHtR 1.03 1.0–1.10 0.206 6.56 0.7103 1.78 0.0011
BMI
+
WC 1.02 0.97–1.08 0.341 7.55 0.7104 1.79 0.0000
BMI
+
PI
1.26 1.09–1.45 0.002 13.58 0.6963 0.22 0.0258
Model 2
BMI
1.06 1.02–1.10 0.002
0.8301 0.00
BMI
+
WHtR 1.04 0.99–1.09 0.142 1.90 0.8319 0.22 0.1850
BMI
+
WC 1.03 0.98–1.08 0.302 2.87 0.8373 0.86 0.0206
BMI
+
PI
1.17 1.01–1.36 0.037 9.87 0.8399 1.17 0.0381
Female
Model 1
BMI
1.07 1.04–1.10 0.000
0.6221
BMI
+
WHtR 1.05 1.01–1.10 0.023 1.89 0.6238 0.27 0.4532
BMI
+
WC 1.06 1.0–1.09 0.034 0.94 0.6245 0.39 0.2316
BMI
+
PI
1.14 1.01–1.29 0.027 6.34 0.6202 0.31 0.2527
Model 2
BMI
1.01 0.98–1.05 0.400
0.7468
BMI
+
WHtR 1.02 0.98–1.07 0.359 0.99 0.7477 0.12 0.6346
BMI
+
WC 1.02 0.97–1.06 0.450 0.99 0.7465 0.04 0.8587
BMI
+
PI
1.04 0.94–1.16 0.437 2.93 0.7474 0.08 0.5754
PR, prevalence ratio; BMI, body mass index; WHtR, waist–height ratio; WC,
waist circumference; PI, ponderal index.
Model 1 was crude while model 2 was adjusted for factors such as age, gender,
smoking, alcohol consumption and physical activity.
% change in PR
=
100
×
absolute [ln (PR
BMI
/PR
testvariables
)]; test variables were BMI
+
WC, BMI
+
WHtR, or BMI
+
PI.
28
% change in AUC
=
100
×
absolute [ln (AUC
BMI
/AUC
testvariables
)]; test variables were
BMI
+
WC, BMI
+
WHtR, or BMI
+
PI.
28
Table 6. Cut-off points for anthropometric indices in predicting
hypertension and prehypertension
Hypertension
Prehypertension
Male
Female
Male
Female
BMI
Cut-off point
24.49
24.44
23.62
28.01
Sensitivity
72.92
74.11
64.65
31.05
Specificity
60
48.9
64.79
58.51
Youden index J
0.33
0.20
0.29
0.20
WHtR
Cut-off point
0.55
0.508
0.50
0.60
Sensitivity
48.96
81.25
58.59
25.79
Specificity
83
40.38
61.97
93.68
Youden index J
0.33
0.22
0.21
0.2
WC
Cut-off point
91.44
96.52
82.55
96.52
Sensitivity
53.13
40.18
71.21
32.11
Specificity
81.47
76.65
50.7
86.21
Youden index J
0.35
0.17
0.22
0.18
PI
Cut-off point
14.45
16.38
13.69
17.65
Sensitivity
70.83
57.65
71.21
28.42
Specificity
57.65
67.3
57.75
87.36
Youden index J
0.28
0.24
0.30
0.16
BMI, body mass index; WHtR, waist–height ratio; WC, waist circumference; PI,
ponderal index.
Table 5. Prevalence ratios corresponding to one standard
deviation increase in anthropometric measures
Anthropometric
index
Hypertension
Prehypertension
PR 95% CI
p
-value PR 95% CI
p
-value
Model 1
WHtR
1.44 1.3–1.56 0.000 1.15 1.08–1.22 0.000
WC
1.41 1.28–1.56 0.000 1.2 1.13–1.27 0.000
BMI
1.35 1.24–1.47 0.000 1.21 1.15–1.27 0.000
PI
1.32 1.21–1.44 0.000 1.17 1.11–1.23 0.000
Model 2
WHtR
1.15 1.01–1.30 0.030 1.04 0.97–1.11 0.258
WC
1.15 1.03–1.29 0.017 1.11 1.03–1.19 0.002
BMI
1.14 1.01–1.27 0.028 1.11 1.04–1.10 0.001
PI
1.12 0.99–1.27 0.063 1.067 1.00–1.14 0.038
PR, prevalence ratio; WHtR, waist–height ratio; WC, waist circumference;
BMI, body mass index; PI, ponderal index.
Model 1 was crude while model 2 was adjusted for factors such as age, smoking,
alcohol consumption and physical activity.

















