
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 3, May/June 2018
152
AFRICA
were NYHA functional class II. Four patients were on medical
treatment with diuretics (furosemide) and anti-remodelling
therapy (spironolactone, carvedilol, enalapril) for previous heart
failure secondary to MR. Eight patients were on diuretics alone.
In this study, LGE was present in four (18%) patients
with CRMR (Table 2). A varied pattern of LGE of the LV
myocardium was noted. These included (1) transmural LGE in
the lateral wall, (2) patchy areas of LGE in the basal septum,
mid-septum and basal inferior wall, (3) transmural fibrosis of
the inferior wall, and (4) sub-epicardial LGE in one patient. The
two patients with transmural involvement had normal coronary
angiograms (done as part of their surgical work-up).
PIIINP and PIP were not elevated in patients compared
to controls. PIIINP concentrations were 11.8 (6.9–21.6) vs
15.7 (13.6–18.5) ng/ml (
p
=
0.09), while PIP levels were 780.4
(727.3–1263.7) vs 1065.1 (589.2–1252.0) µg/ml (
p
=
0.13) (Table
3). Log MMP-1 was elevated in patients with CRMR compared
to the controls (3.45
±
0.7 vs 2.7
±
0.9,
p
=
0.02). There was no
difference in log TIMP-1 between CRMR patients and controls
(4.6
±
0.39 vs 4.8
±
0.30,
p
=
0.15). The ratio of log MMP-1 to
TIMP-1 was increased (–1.2
±
0.6 vs –2.1
±
0.89,
p
=
0.002) in the
study patients compared to the controls.
Discussion
The main findings of this study were: fibrosis, as assessed by
LGE was uncommon in CRMR; and biomarkers suggestive
of collagen degradation (MMP-1, MMP-1/TIMP-1 ratio) were
increased in CRMR, but no changes in biomarkers of collagen
synthesis (PIP and PIIINP) were noted.
In this study, the majority of patients with CRMR did not
have LV myocardial fibrosis on LGE. There are no studies on
CRMR to draw comparisons from, but the limited studies done
in degenerative MR have shown the presence of fibrosis on LGE
in about 30% of patients compared to only 18% in the current
study.
4,26
In contrast with our study, biological factors such as
advanced age, and co-morbidities such as hypertension and
diabetes may have contributed to the higher prevalence of fibrosis
in these studies.
4,26
Furthermore, one study used T1 mapping in
addition to LGE, and was able to report on microvascular
fibrosis, increasing the detection rate of fibrosis in their study.
4
An alternative explanation for a lack of fibrosis in the majority
of patients in this study may be the presence of diffuse fibrosis,
which is missed by the LGE technique, as it compares regions
of normal myocardium to abnormal myocardium.
1
Conversely,
fibrosis may indeed have been absent, and this is supported by
the normal markers of collagen synthesis in this study.
The above hypothesis is further supported on the basis of
a study done by Ho
et al
. in hypertrophic cardiomyopathy
patients, where it was noted that a pro-fibrotic state (as assessed
by increased biomarkers of synthesis) preceded the development
of fibrosis visible on MRI.
27
The sample size in our study was
too small to draw comparisons based on the presence or absence
of LGE, or to comment on patterns of enhancement in detail.
Interestingly though, LV fibrosis in the four patients was not
confined to the posterobasal region, an area noted to be affected
more commonly by rheumatic fever.
7
A higher prevalence of fibrosis is observed commonly in
pressure-overload states such as aortic stenosis.
2
The exact
mechanism of greater fibrosis in pressure-overload states
compared to volume-overload states remains speculative.
28
The
following reasons have been proposed: (1) a greater supply/
demand mismatch in pressure-overload states resulting in
ischaemia and fibrosis; (2) data from animal studies have shown
that pro-fibrotic pathways are activated to a larger extent in
pressure-overload states compared to volume-overload states; (3)
the predominant pathology in MR may be extracellular volume
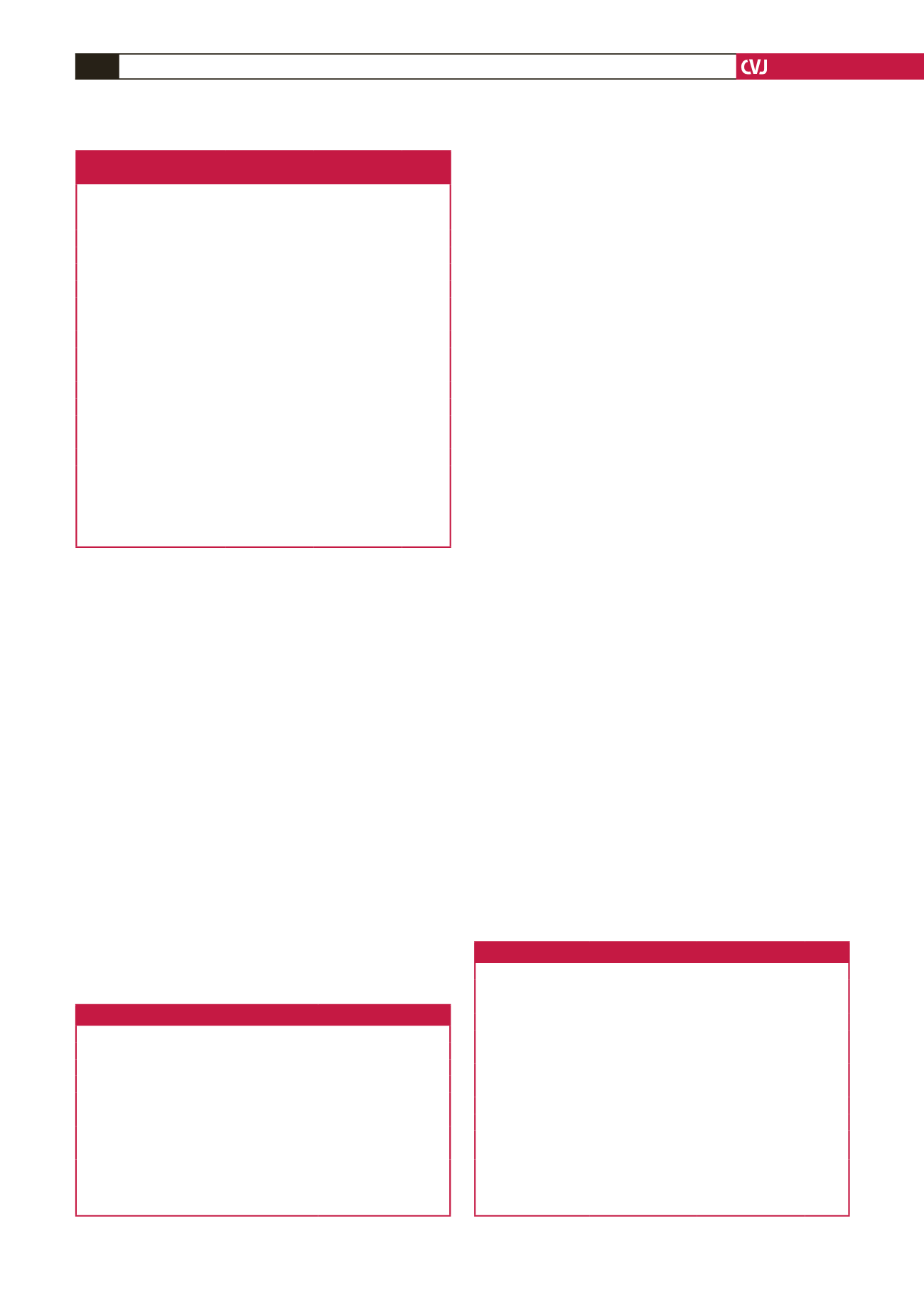
Table 1. Clinical and echocardiographic characteristics
of the study patients and controls
Variable
Study group
(
n
=
22)
Control
(
n
=
14)
p
-value
Clinical parameters
Age (years)
36.3
±
13.9
40.3
±
14.2
0.40
Gender (F:M)
18:4
10:4
0.36
SBP (mmHg)
123.2
±
9.5
122.9
±
5.1
0.91
DBP (mmHg)
77.2
±
6.4
74.6
±
12.3
0.34
Pulse (beats/min)
74.6
±
13.1
75.5
±
13.3
0.55
Body mass index (kg/m
2
)
24.8
±
4.7
28
±
5.7
0.06
Body surface area (m
2
)
1.6
±
0.2
1.7
±
0.2
0.24
Echocardiographic parameters
LVEDD (mm)
56.2
±
7.4
42.2
±
6.1
<
0.001
LVESD (mm)
41.5
±
8.6
26.7
±
4.0
<
0.001
EDVi (ml/m
2
)
†
90.4 (71.5–103.8) 43.2 (35.2–43.2)
<
0.001
ESVi (ml/m
2
)
†
39.6
±
19.6
15.3
±
4.6
0.001
LVEF (%)
59.8
±
10.6
60.6
±
17.1
0.5
LV mass index (g/m
2
)
†
100.1
±
33.8
61.4
±
18.7
0.004
†
Data are presented as median (interquartile range), mean
±
SD or %. Values
are indexed to BSA.
DBP: diastolic blood pressure; SBP: systolic blood pressure; LV: left ventricle;
EDD: end-diastolic diameter; ESD: end-systolic diameter; EDVi: end-diastolic
volume indexed; ESVi: end-systolic volume indexed; LVEF: left ventricular
ejection fraction.
Table 2. CMR characteristics of the study patients
CMR characteristics
Values
Regurgitant volume (ml)
47.0
±
19.9
Regurgitant fraction (%)
49.2 (31.7–56.2)
EDVi (ml/m
2
)
†
98.5 (81–111.1)
ESVi (ml/m
2
)
†
49.1
±
36.7
LVEF (%)
58.8
±
15.1
Moderate MR,
n
(%)
9 (41)
Severe MR,
n
(%)
13 (55)
†
Data are presented as median (interquartile range), mean
±
SD or %. Values
are indexed to BSA.
EDVi: end-diastolic volume indexed; ESVi: end-systolic volume indexed; LVEF:
left ventricular ejection fraction; MR: mitral regurgitation.
Table 3. Biomarkers in the study patients compared to controls
Biomarkers
Study group (
n
=
22) Control (
n
=
14)
p
-value
PIIINP (ng/ml)
11.8 (6.9-21.6)
15.7 (13.6-18.5)
0.09
Log PIIINP
2.5
±
0.7
2.7
±
2.6
0.18
PIP (µg/ml)
780.4 (727.3–1263.7) 1065.1 (589.2–1252.5) 0.13
Log PIP
6.79
±
0.57
6.8
±
0.47
0.29
MMP-1 (ng/ml)
37.5 (19.9–59.7)
16.2 (6.53–37.9)
0.3
Log MMP-1
3.45
±
0.7
2.7
±
0.9
0.02
TIMP-1 (ng/ml)
95.4 (90.4–140.1)
139.2 (110.3–155.5)
0.1
Log TIMP-1
4.6
±
0.4
4.8
±
0.30
0.15
MMP-1/TIMP-1 ratio 0.26 (0.21–0.43)
0.11 (0.07–0.26)
0.08
Log MMP-1/TIMP-1
ratio
–1.2
±
0.6
–2.05
±
0.89
0.002
Data are presented as median (interquartile range), mean
±
SD or %.
PIIINP: procollagen III N-terminal pro-peptide; PIP: procollagen type IC
peptide; MMP: matrix metalloproteinase; TIMP: tissue inhibitor of matrix
metalloproteinase.

















