
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 3, May/June 2018
168
AFRICA
Mean mitral valve area, measured by planimetry on
transoesophageal echocardiography (TEE), was 0.69
±
0.13 cm
2
(range 0.5–0.9). Mean transmitral diastolic gradient was 24.1
±
5.9 mmHg (range 16–35) and mean estimated pulmonary artery
systolic pressure was 110.0
±
35 mmHg (75–170). Other baseline
characteristics of the patients are shown in Table 1.
Under general anaesthesia, right femoral vein access was
taken with a 7F short sheath. A 0.025-inch regular wire was
advanced up the superior caval vein and a 7F long sheath was
advanced to the left innominate vein. The wire was withdrawn
and a Brockenbrough needle (Medtronic Inc, Minneapolis, MN,
USA) was introduced.
After sliding the system down to the oval fossa, transseptal
puncture was performed under TEE and single-plane fluoroscopy
guidance. The needle was withdrawn into the dilator and the
sheath–dilator assembly was advanced into the left atrium. Once
in the left atrium, the dilator was removed.
A 6F 110-cm-long wedge balloon catheter (Arrow Int, Inc,
Bernville Rd, Reading PA, USA) was advanced into the left
atrium. The pre-formed stiff end of a regular wire (Fig. 1)
was used as a stylet to guide the inflated wedge balloon across
the mitral valve. Once the balloon was at the apex of the left
ventricle, its position at the centre of the mitral apparatus (and
not through the chordae) was confirmed by TEE.
The wedge balloon catheter was then advanced up the
ascending aorta, using the pre-shaped end of the stiff wire, if
necessary. A 0.035-in
×
260-cm Terumo wire (Terumo Medical
Corporation, Cottontail Lane, Somerset, New Jersey, USA) was
advanced through the wedge catheter and the wire was snared
to the descending aorta from the arterial side to establish an
arteriovenous loop (Fig. 2A). Then the inflated wedge catheter
was again withdrawn into the left ventricle and pushed and
pulled gently through the mitral valve apparatus to ascertain that
there was no entrapment within the mitral valve chordae. The
wedge balloon and the long sheath were then removed.
A 12F to 14F short sheath was introduced into the femoral
vein. The septal puncture was dilated with a 6- or 8-mm balloon
(Fig. 2A). Finally, a Nucleus balloon (NuMED Canada Inc,
Second Street West Cornwall, ON, Canada) of appropriate
size, according to the patient’s size and TEE measurement of
the mitral annulus, was introduced and placed across the mitral
valve. We did not encounter any difficulty with passing the
balloon through the septal puncture in any of our patients.
A 20-cm
3
syringe with 25% contrast and 75% saline
combination was attached using a three-way stopcock. An
inflation device filled with a similar combination of contrast and
saline was attached. The desired inflation pressure was decided
based on the table provided with the balloon (Table 2), in order to
achieve the exact target diameter. Both ends of the arteriovenous
loop were pulled to stabilise the balloon in a good position and
the balloon was inflated using fluoroscopic and TEE guidance.
Table 1. Baseline characteristics of patients treated for severe
rheumatic mitral stenosis using a modified Nucleus balloon technique
Variables
Mean
±
SD (range)
Age (years)
14.3
±
4.2 (12–26)
Weight (kg)
30.3
±
7.4 (23–48)
Height (cm)
146.6
±
9.9 (133–163)
Spontaneous echo contrast in the left atrium
(number of patients)
5
NYHA functional class
Class I
–
Class II
3
Class III
8
Class IV
–
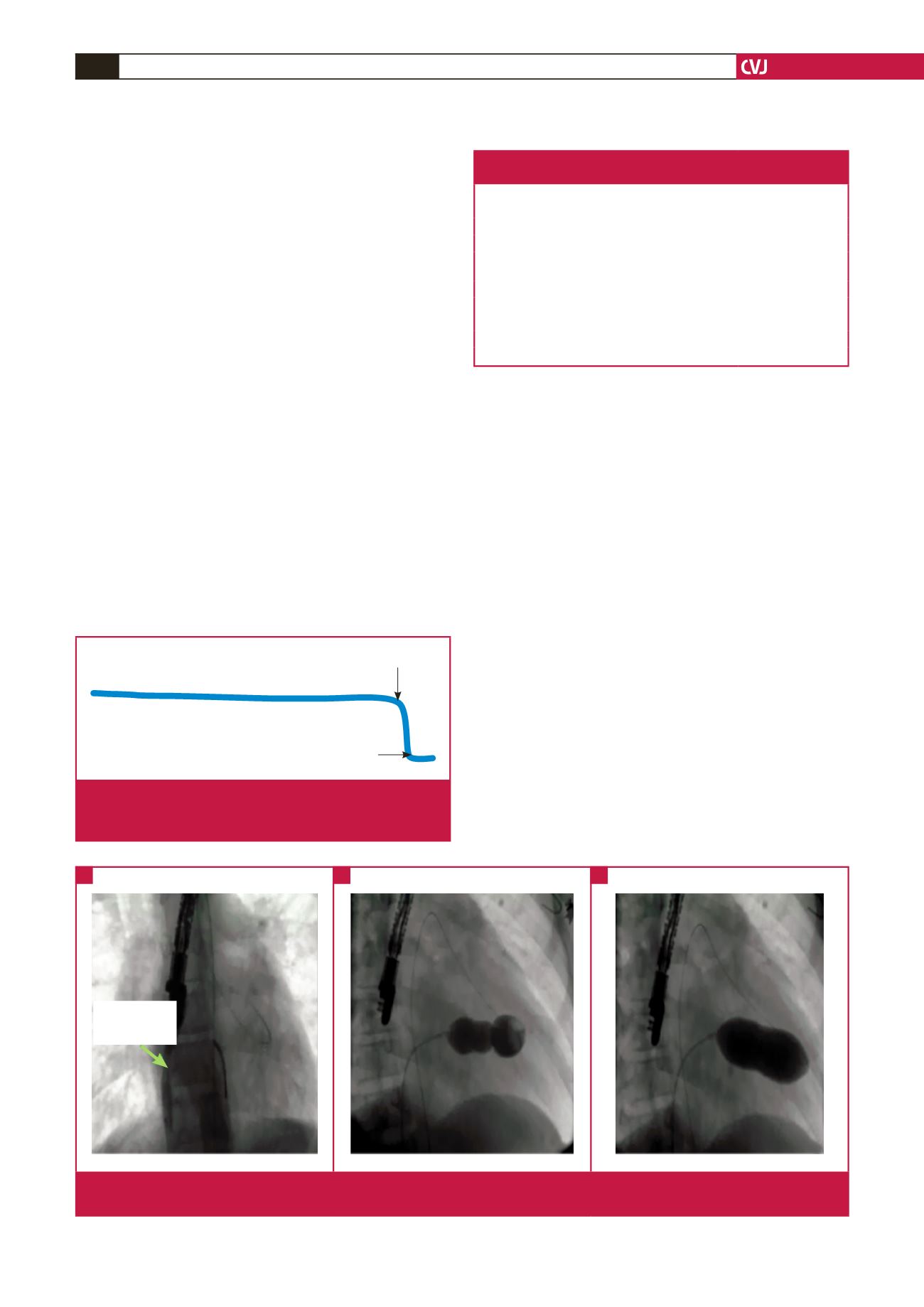
Mitral valve curve
septal curve
Fig. 1.
Pre-shaped stiff end of a regular guide wire with septal
and mitral valve cuves for guiding the wedge balloon
across the mitral valve
A 6-mm balloon
across septal
puncture
Fig. 2.
A. Establishment of arteriovenous loop and dilation of the septal puncture. B. Nucleus balloon inflated across a severely
stenotic mitral valve. C. Full inflation of the Nucleus balloon across the mitral valve showing near-disappearance of the waist.
A
B
C

















