
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 4, July/August 2018
226
AFRICA
National Hospital, a major public referral centre, to evaluate the
presentation, management and outcomes of patients with ACS.
Methods
FromNovember 2016 to April 2017 we conducted a retrospective
chart review of ACS cases managed at Kenyatta National
Hospital from 2013 to 2016. We used the existing electronic
disease code database to identify ACS cases, using primary
discharge codes (I20-I24) from the World Health Organisation
International Classification of Diseases (ICD-10) system.
5
The diagnosis of ACS subtype was made by the primary
treating physician at the time of the index hospitalisation, based
on the Third Universal Definition of Myocardial Infarction.
6
We excluded cases that had a primary diagnosis of ACS, but
upon further review of the medical admission, most likely had
myocardial infarction secondary to a non-ACS aetiology (i.e. a
non-type 1 myocardial infarction). In cases that the ACS subtype
was not directly specified in the medical record, the primary data
extractor (EB) reviewed each clinical presentation, biomarkers
and ECG findings and determined the ACS subtype based on
the Third Universal Definition of Myocardial Infarction.
6
We included adults over 18 years with a diagnosis of ACS
admitted and managed between 2013 and 2016. We abstracted
demographics, presentation, self-reported medical history,
diagnostics, treatment data and in-hospital clinical events. We
used combined paper and electronic data-capture systems to
abstract data from the medical record, which was performed by
one author (EB).
We defined guideline-directed in-hospital medical therapy as
receiving a combination of aspirin, a second antiplatelet (e.g.
clopidogrel, ticagrelor or prasugrel), beta-blocker within 24
hours of presentation and anticoagulation at any point during
the hospitalisation. We defined guideline-directed discharge
medical therapy as receiving a combination of aspirin, second
antiplatelet drug, beta-blocker and statin. We assessed in-hospital
outcomes, including in-hospital death and in-hospital major
adverse cardiovascular events (MACE), defined as the composite
of in-hospital death, re-infarction, stroke, heart failure, major
bleeding or cardiac arrest.
We acquired ethics approval to conduct this research from
the Kenyatta National Hospital and University of Nairobi
ethics research committee (KNH-UON ERC), Northwestern
University institutional review board, and University of
Washington institutional review board. Informed consent was
waived based on the retrospective nature of the study for the
collection of anonymised data.
Statistical analysis
We present continuous data as means (standard deviation)
or median (range or interquartile range) when skewed, and
categorical data as proportions. Comparisons by ACS subtype
were made via analysis of variance for continuous variables
and chi-squared testing for categorical variables. We created
multivariable logistic regression models using the Global Registry
of Acute Coronary Events (GRACE) risk score to evaluate
the association between clinical variables, including guideline-
directed medical therapy and in-hospital death or major adverse
cardiovascular events.
4
We defined statistical significance using a
two-sided
p
-value
<
0.05. We used Stata version 14.0 (StataCorp,
LLC. College Station, TX).
5
Results
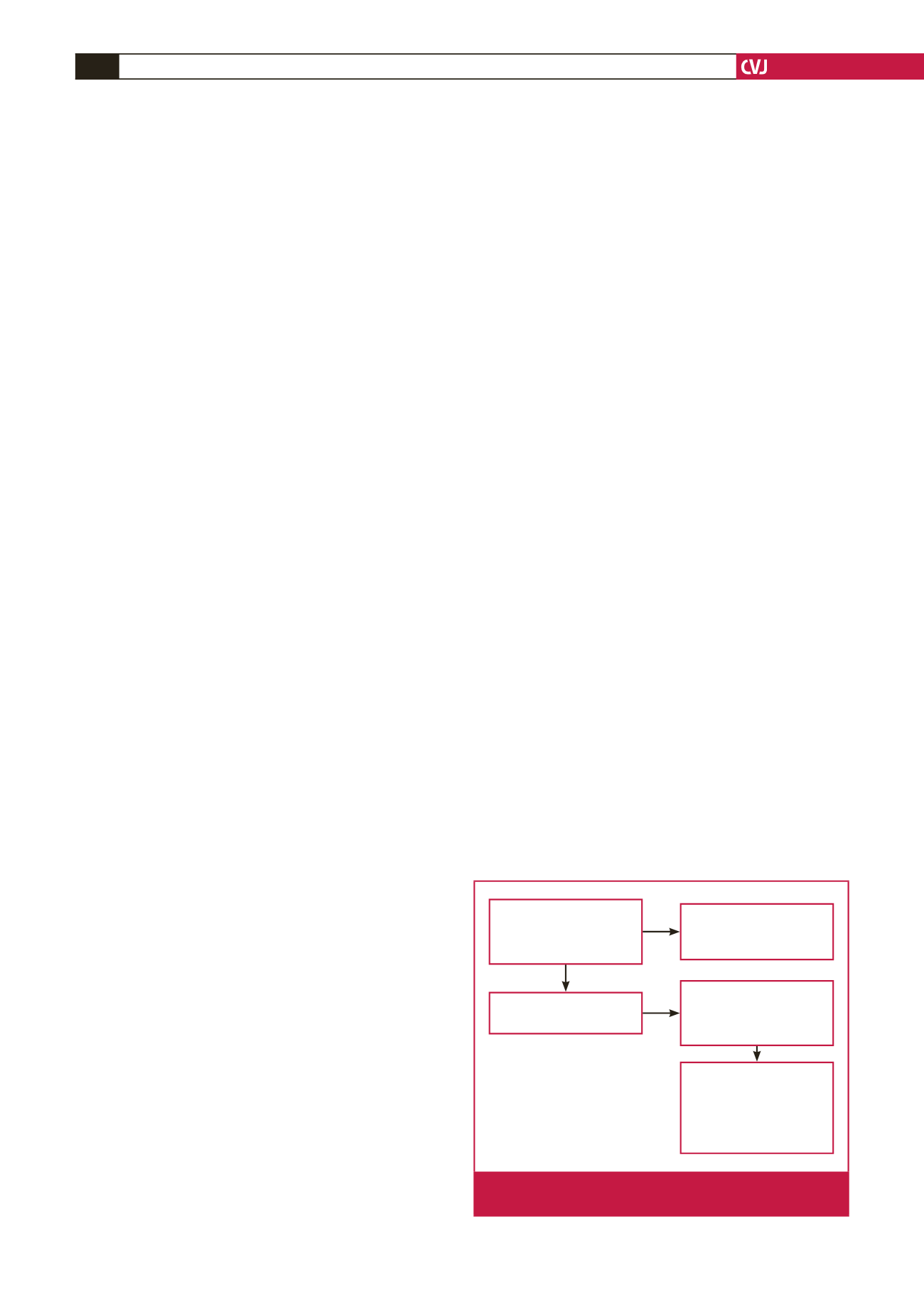
Fig. 1 demonstrates the flow of participants in this study. We
identified a total of 330 admissions that met our study criteria.
We could only retrieve partial admission data from 2013 due to
a hospital-wide electronic database loss that occurred between
2011 and 2013, which led to the exclusion of 51 cases. A further
81 cases were excluded because of incorrect diagnosis (20)
or ACS not being the primary discharge diagnosis (61). We
therefore included 196 cases in our final analysis.
Table 1 summarises patients’ baseline characteristics by ACS
subtype. The majority (57%) of the cases were ST-elevation
myocardial infarction (STEMI) followed by non-ST-elevation
myocardial infarction (NSTEMI, 26%) and unstable angina
(UA, 12%). Cases without an ECG but with positive biomarkers
and clinical presentation consistent with ACS represented 5% of
cases. Most participants (64%) were men, and the median age
(IQR) was 58 (48–68) years. More than one-third (38%) of all
admissions were transferred from an outside hospital.
Hypertension (63%) was the most common co-morbidity,
followed by diabetes (41%). Smoking rates were low across all
groups (9%); however, 27% had undocumented smoking status,
which likely led to underestimation of the overall smoking
prevalence. The proportion of patients who presented in heart
failure with Killip class
>
1 was highest among STEMI cases
(44%).
Table 2 shows a summary of the in-hospital management
of ACS patients. We stratified the data into four groups: key
investigations, in-hospital acute medical therapy focusing on
administration of guideline-directed medications within the
first 24 hours of admission, in-hospital reperfusion therapy, and
discharge medical therapy.
Overall, 82% of all cases received an ECG within 24 hours
of presentation, with higher rates among patients who were
transferred versus non-transfer patients (88 vs 71%,
p
<
0.001).
The proportion of patients that received an ECG within 24
hours of admission each year between 2013 and 2016 was 82,
51 charts not available
due to hospital-wide
electronic database loss
330 cases identified
through electronic data-
base search with WHO
ICD-10 code I20-I24
81 cases excluded:
20 wrong diagnoses
61 ACS not the primary
diagnosis
Retrieved charts
for 277 cases
196 cases included in
final analysis
2016: 68 cases
2015: 50 cases
2014: 50 cases
2013: 28 cases
Fig. 1.
Study flow chart of ACS cases admitted to Kenyatta
National Hospital between 2013 and 2016.

















