
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 4, July/August 2018
228
AFRICA
antiplatelet, beta-blocker within 24 hours of admission and an
anticoagulant at some point during the hospitalisation was 56%.
Aminority of overall (17 cases, 9%) andSTEMI cases (12 cases,
11%) underwent in-hospital diagnostic cardiac catheterisation
with only 12% undergoing percutaneous coronary intervention
(one NSTEMI, one unstable angina). Using the 2013 American
College of Cardiology/American Heart Association guidelines
for the management of STEMI,
7
we identified 37 (33%) STEMI
cases eligible for reperfusion, half of whom were transfers. Two
eligible STEMI cases (5%) received thrombolytic therapy and
both were transferred from outside hospitals.
We assessed discharge medical therapy, focusing on guideline-
directed prescription of medications upon discharge and
excluding patients who left against medical advice (
n
=
4).
Discharge aspirin use was 96%, and second antiplatelet agent
discharge use was 82%; combined dual antiplatelet use was
81%. Beta-blocker discharge use was 70%, and statin discharge
use was 86%. The rate of guideline-directed discharge medical
therapy defined as receiving aspirin, a second antiplatelet
and beta-blocker therapy was also 56%. Among individuals
with an ejection fraction less than 40% (
n
=
33), 63% received
an ACE inhibitor or angiotensin receptor blocker (ARB).
Among patients with ejection fraction less than 40%, the rate
of guideline-directed medical therapy with simultaneous dual
antiplatelet, beta-blocker, statin and ACE inhibitor or ARB use
was 48%.
The overall in-hospital mortality rate was 17%, with a
gradient in mortality rate by ACS subtype (STEMI 21%,
NSTEMI 10%, UA 9%, biomarker positive only 30%,
p
=
0.16)
(Table 3). The rate of MACE, defined as death, re-infarction,
stroke, cardiogenic shock, major bleeding or cardiac arrest was
40%, with a similar gradient by ACS subtype (STEMI 54%,
NSTEMI 20%, UA 7%, biomarker positive only 30%,
p
<
0.001)
(Table 3).
Table 4 summarises variables assessed as potential predictors
of in-hospital mortality before and after adjustment using the
GRACE risk score. After multivariable adjustment, higher
serum creatinine level was associated with higher odds of
in-hospital death (OR
=
1.84, 95% CI: 1.21–2.78), and Killip
class
>
1 was associated with in-hospital composite of death,
re-infarction, stroke, major bleeding or cardiac arrest (STEMI:
OR
=
4.71, 95% CI: 2.46–9.02; Killip
>
1: OR
=
10.7, 95% CI:
3.34–34.6).
We also evaluated the association between receiving guideline-
directed in-hospital medical therapy and in-hospital MACE
level using logistic regression and adjusting for covariates in
the GRACE risk score. We did not demonstrate an association
between in-hospital death and combined in-hospital death and
MACE before and after multivariable adjustment (OR
=
0.77,
95% CI: 0.27–2.20; OR
=
1.88, 95% CI: 0.86–4.10, respectively),
but these results were imprecise and were likely driven by the
small sample size and number of events.
Discussion
Through this retrospective chart review we report the
presentation, management and outcomes of ACS patients
managed at Kenyatta National Hospital between 2013 and 2016.
Most patients were men in their late 50s presenting with STEMI.
Approximately one out of every five patients did not receive an
ECG within the first 24 hours, and one out of every 20 patients
did not receive an ECG at all. While more than one out of every
two patients received echocardiography, the gap in ECG care
represents an opportunity for diagnostic improvement. Rates of
in-hospital medical therapy were relatively high but reperfusion
rates among eligible individuals were low. Increasing timely,
appropriate reperfusion therapy for eligible STEMI patients may
be an important area of focus because of the high mortality rate
demonstrated among these patients.
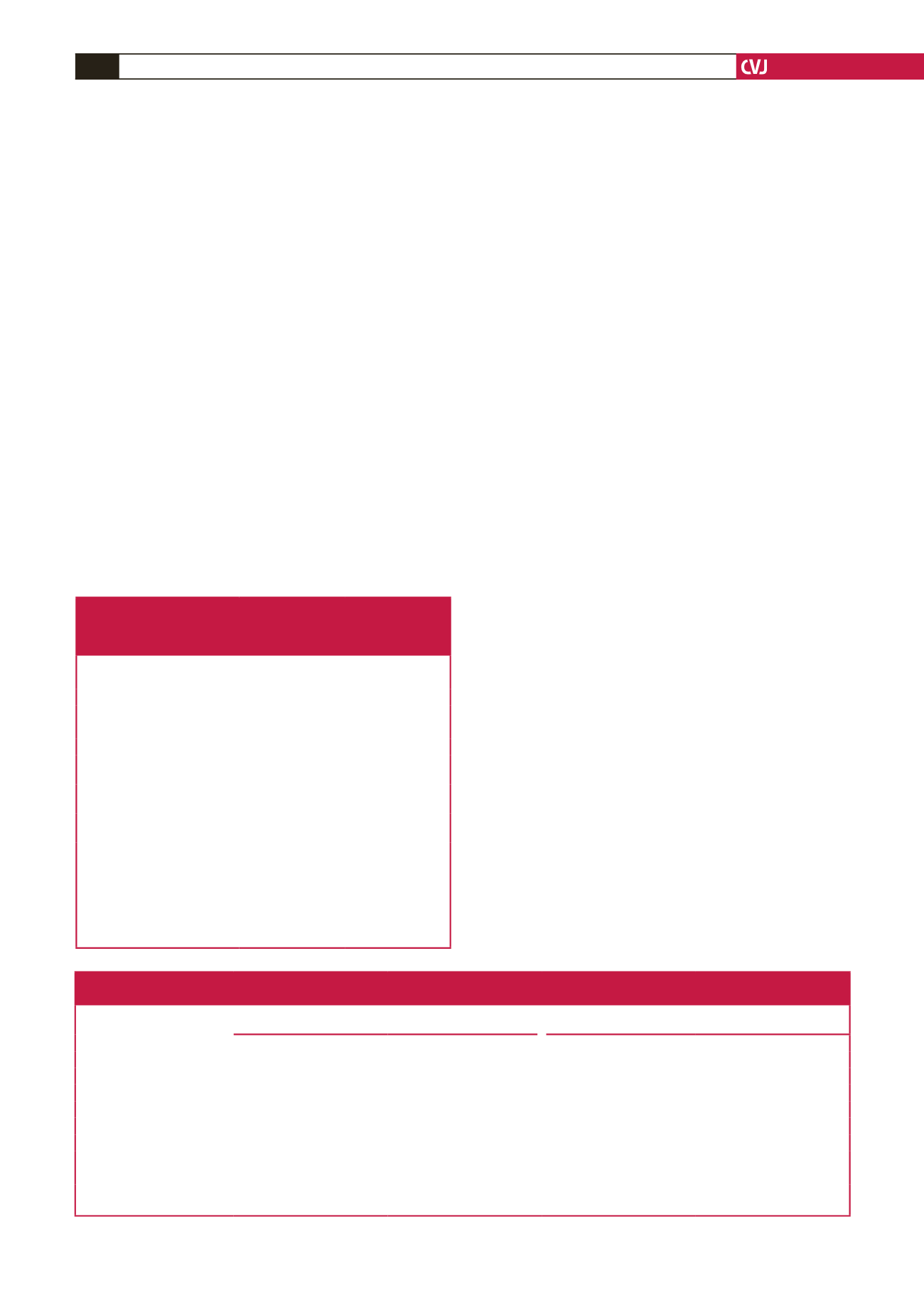
Table 4. Predictors of in-hospital death and major adverse cardiovascular events (MACE) including death, re-infarction, stroke, heart failure,
cardiogenic shock, major bleeding and cardiac arrest of ACS patients admitted to Kenyatta National Hospital between 2013 and 2016
Unadjusted OR (95% CI)
Adjusted (for age, gender and GRACE risk score variables)
OR (95% CI)
Variables
In-hospital death,
n
=
33
In-hospital MACE,
n
=
78
In-hospital death,
n
=
33
In-hospital MACE,
n
=
78
Age (per year)
1.03 (1.0–1.06)*
1.00 (1.01–1.05)*
1.04 (0.98–1.11)
1.01 (0.98–1.06)
Heart rate (per bpm)
0.98 (0.97–1.00)
1.00 (0.99–1.02)
1.02 (0.99–1.11)
1.01 (098–1.04)
SBP (per mmHg)
0.99 (0.98–1.00)
0.99 (0.98–1.00)
0.96 (0.93–0.98)
0.98 (0.96–0.99)
Serum Cr (per mg/dl)
1.35 (1.12–1.66)*
1.13 (0.94–1.34)
1.84 (1.21–2.78)*
1.04 (0.84–1.31)
Killip class 1 vs
>
1
5.80 (2.5–13.7)*
11.45 (0.80–22.4)*
1.8 (0.42–8.14)
10.7 (3.34–34.6)*
Positive cardiac enzyme
2.60 (0.58–11.8)
2.23 (0.89–5.63)
0.91 (0.94–8.80)
1.42 (0.35–5.73)
ST-segment deviation
2.11 (0.85–5.22)
5.35 (2.60–10.99)*
3.12 (0.57–16.87)
1.72 (0.12–24.40)
STEMI vs UA (ref)
2.84 (062–2.98)
8.37 (2.36–29.70)*
0.77(0.02–38.56)
1.71 (0.21–13.80)
*
p
-value
<
0.05; GRACE risk score variables: age, gender, SBP, HR, positive cardiac enzyme, ST-segment change, creatinine, cardiac arrest.
SBP: systolic blood pressure, HR: heart rate, Cr: creatinine, STEMI: ST-segment myocardial infarction.
Table 3. In-hospital mortality and major adverse cardiovascular events
and association between in-hospital guideline-directed therapy and
in-hospital outcomes of ACS patients admitted and managed at
Kenyatta National Hospital between 2013 and 2016
In-hospital mortality In-hospital MACE
All,
n
(%)
33 (17)
78 (40)
STEMI,
n
(%)
23 (21)
61 (54)
NSTEMI,
n
(%)
5 (10)
11 (22)
UA,
n
(%)
2 (8)
3 (13)
BM (+) only
3 (30)
3 (30)
*Guideline-directed in-hospital
medical therapy,
n
(%)
8 (12)
27 (40)
Non-guideline-directed in-hospi-
tal medical therapy,
n
(%)
8 (15)
14 (26)
Guideline-directed vs non-guide-
line-directed, OR (95% CI)
0.76 (0.27–2.20)
1.88 (0.86–4.10)
ACS: acute coronary syndrome, STEMI: ST-elevation myocardial infarction,
NSTEMI: non-ST-elevation myocardial infarction, UA: unstable angina, BM
(+): biomarker positive only: these are cases that presented with symptoms of
ACS and had a positive biomarker test, however did not get an ECG during
their hospitalisation, MACE: major adverse cardiovascular events.
*Guideline-directed in-hospital medical therapy includes patients who received
aspirin, a second antiplatelet and a beta-blocker within 24 hours of presentation
and an anticoagulant at any point during hospitalisation.

















