
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 4, July/August 2018
AFRICA
227
80, 80 and 72%, respectively (
p
=
0.69). Cardiac biomarkers
were measured in 86% of cases, and approximately half (52%)
received echocardiography during their hospitalisation. A total
of 10 cases were primarily diagnosed by symptoms and positive
biomarkers without an ECG, with six of these cases managed in
2016, three in 2015, one in 2014 and none in 2013.
During the acute management phase, dual antiplatelet use
was 87%. The rates of beta-blocker use (72%) within the
first 24 hours of admission and anticoagulant use (72%; 80%
enoxaparin) during hospitalisation were also relatively high.
After excluding transfer patients, the rate of guideline-directed
in-hospital medical therapy, defined as receiving aspirin, a second
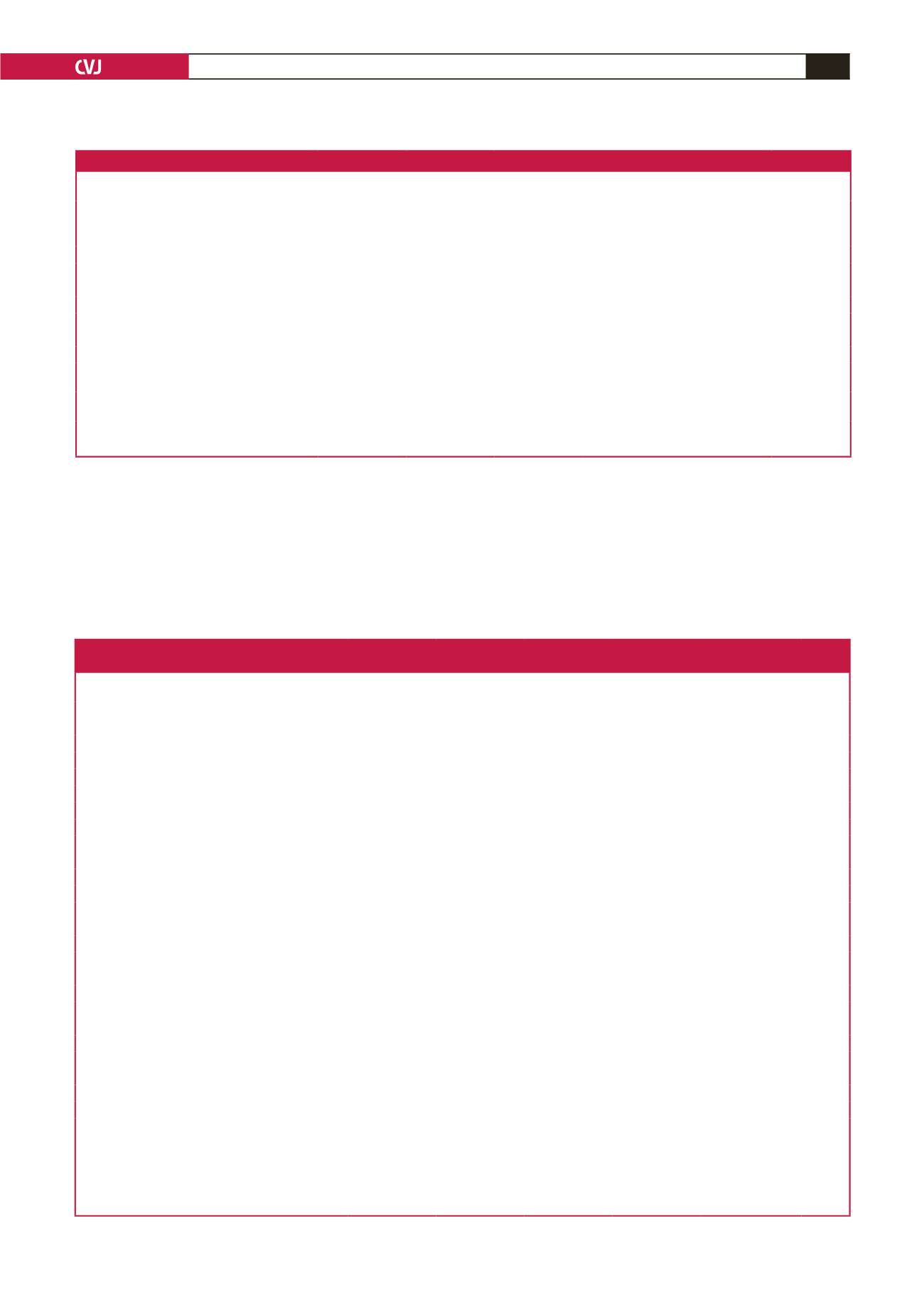
Table 1. Basic characteristics of patients admitted with ACS at Kenyatta National Hospital between 2013 and 2016 by ACS subtype
Variables
All
n
=
196
STEMI
n
=
112
NSTEMI
n
=
50
UA
n
=
24
Biomarker (+) only
n
=
10
p
-value
Type of ACS
196
112 (57)
50 (26)
24 (12)
10 (5)
Age, years
(median, IQR)
57.5
(48, 68)
60
(53, 69)
56.5
(44, 68)
51.5
(48, 67)
62.5
(45, 65)
0.18
Male,
n
(%)
127 (65)
81 (65)
31 (24)
9 (8)
6 (5)
0.01
Transferred,
n
(%)
74 (38)
56 (50)
11 (22)
5 (21)
2 (20)
<
0.001
History of hypertension,
n
(%)
124 (63)
67 (60)
34 (680
18 (75)
5 (50)
0.34
History of diabetes,
n
(%)
80 (41)
53 (47)
16 (32)
9 (38)
2 (20)
0.14
History of stroke,
n
(%)
1 (0.5)
1 (0.9)
0
0
0
0.86
History of end-stage renal disease,
n
(%)
4 (2)
0
2 (4)
2 (8)
0
0.03
History of smoking,
n
(%)
17 (9)
13 (12)
3 (6)
1 (4)
0
0.07
Heart rate, bpm
(median, IQR)
84
(72–101)
84
(72–103)
86
(100–73)
90
(95–76)
79
(66–101)
0.79
Systolic blood pressure, mmHg
(median, IQR)
137
(116–156)
136
(114–155)
143
(116–156)
138
(103–156)
150
(132–172)
0.41
Killip class
>
1,
n
(%)
73 (39)
50 (44)
17(34)
5 (21)
5 (50)
0.07
STEMI: ST-elevation myocardial infarction, NSTEMI: non-ST-elevation myocardial infarction, UA: unstable angina, bpm: beats per minute.
Table 2. In-hospital and discharge diagnostics, medical and reperfusion therapy, and rates of guideline-directed in-hospital
and discharge medical therapy of ACS patients admitted to Kenyatta National Hospital between 2013 and 2016
Variables
All
n
=
196
STEMI
n
=
112
NSTEMI
n
=
50
UA
n
=
24
Biomarker (+) only
n
=
10
p
-value
Key investigations
ECG
<
24 h,
n
(%)
152 (78)
95 (85)
37 (74)
20 (83)
–
<
0.001
Non-transferred
87 (71)
43 (77)
29 (74)
15 (79)
–
Transferred
65 (84)
52 (93)
8 (73)
5 (100)
–
Cardiac enzyme (+) in 24 h,
n
(%)
134 (68)
75 (67)
49 (98)
–
9 (90)
<
0.001
Echocardiography,
n
(%)
101(52)
61 (54)
28 (56)
10 (42)
2 (20)
0.13
LVEF
<
40%,
n
(%)
33 (33)
25 (41)
6 (21)
2 (20)
0 (0)
<
0.001
In-hospital medical therapy
Aspirin,
n
(%)
185 (94)
104 (93)
50 (100)
22 (92)
–
0.21
Second antiplatelet,
n
(%)
172 (88)
99 (88)
46 (92)
20 (83)
–
0.20
Beta-blocker,
n
(%)
137 (72)
79 (75)
32 (65)
18 (75)
–
0.68
Anticoagulation
140 (72)
85 (76)
38 (76)
15 (65)
–
<
0.001
Guideline-directed in-hospital medical therapy*,
n
(%)
58 (56)
34 (60)
22 (56)
10 (53)
2 (25)
In-hospital reperfusion therapy
Eligible for reperfusion,
n
(%)
–
37 (33)
–
–
–
Thrombolysis,
n
(%)
–
2 (5)
–
–
–
Diagnostic catheterisation,
n
(%)
17 (9)
12 (11)
4 (8)
1 (10)
0 (0)
PCI,
n
(%)
2 (12)
0 (0)
1 (25)
1 (100)
–
CABG,
n
(%)
0 (0)
0 (0)
0 (0)
0 (0)
0 (0)
Medications on discharge
Aspirin,
n
(%)
152 (96)
86 (99)
41 (91)
19 (86)
6 (100)
0.62
Second antiplatelet,
n
(%)
131 (82)
79 (91)
34 (76)
13 (59)
5 (83)
0.07
Beta-blocker,
n
(%)
115 (72)
67 (77)
25 (56)
17 (77)
6 (100)
0.04
Statin,
n
(%)
137 (86)
78 (90)
34 (76)
18 (82)
4 (67)
0.31
ACEI/ARB for LVEF
<
40%,
n
(%)
19 (63)
13 (59)
5 (83)
1 (50)
–
0.41
Guideline directed discharge medical therapy**,
n
(%)
89 (56)
34 (64)
22 (47)
10 (41)
3 (60)
ACS: acute coronary syndrome, STEMI: ST-elevation myocardial infarction, NSTEMI: non-ST-elevation myocardial infarction, UA: unstable angina, Biomarker (+)
only: these are cases that presented with symptoms of ACS and had a positive biomarker test, however did not get an ECG during their hospitalisation, LVEF: left
ventricular ejection fraction, PCI: percutaneous coronary intervention, CABG: coronary artery bypass graft, ACEI: ACE inhibitor, ARB: angiotensin receptor blocker.
*Guideline-directed in-hospital medical therapy includes patients who received aspirin, a second antiplatelet and a beta-blocker within 24 hours of presentation and an
anticoagulant at any point during hospitalisation.
**Guideline-directed discharge medical therapy includes patients who received aspirin, a second antiplatelet, a beta-blocker and a statin at discharge.

















