
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 5, September/October 2019
288
AFRICA
IC administration of tirofiban.
Topol
et al
. showed that tirofiban in comparison with
abciximab provided more platelet inhibition in diabetic patients
during follow up and helped to prohibit PCI-related ischaemic
and thrombotic complications.
25
The theory is to achieve a high
drug concentration in the culprit epicardial vessel and small
vasculature by administering IC tirofiban during PCI. Compared
with IV delivery of tirofiban, IC delivery was associated with
greater procedural success (e.g. TIMI grade 3 flow).
26
Our findings revealed that no reflow and slow flow were
effectively reduced and TIMI flow and MBG had better
outcomes with IC injection of tirofiban. These results were in
concordance with recent studies that proved that IC
27
and intra-
lesional delivery of tirofiban through an aspiration catheter had
better myocardial perfusion and fewer complications, even in
complex PCI.
28
Loss of endothelium-dependent vasodilation, inflammatory
reaction and platelet-dependent micro-thrombosis are enhanced
by hyperglycaemia, thereby aggravating the perfusion disturbance
of coronary microcirculation.
29
The mortality rate was much
higher in patients when MBG decreased to 0 to 1.
6,30
To the best of our knowledge, this is the first study to
demonstrate short-term outcomes and safety of IC injection of
high-dose bolus tirofiban plus a maintenance IV, compared with
IV tirofiban in diabetic patients with STEMI. We showed that
IC tirofiban resulted in decreased inflammation in MI, which
was evidenced by a significant reduction in peak CRP level.
Previous studies have reported on the predictive value of CRP
in determining the risk of future cardiovascular events.
31,32
Other
studies have documented a post-procedure CRP rise in relation
to myonecrosis.
33
The efficient inhibition of platelet aggregation
by tirofiban led to inhibition of inflammatory mediators.
34
In spite of no significant differences in bleeding events and
MACE rates during the 30-day follow up after PCI, the IC tirofiban
group showed an improvement in left ventricular function.
However, we need large, long-term, multicentre, randomised trials
to assess whether IC injection of tirofiban at the time of primary
PCI improves clinical outcome in diabetic patients.
The results of this study have certain limitations. We used
non-random selection of patients for IC tirofiban, the patient
number was relatively small, and we evaluated IC tirofiban on
STEMI but did not compare the effects in NSTE-ACS. Despite
including elderly patients in the study, we did not compare major
and minor bleeding incidence and platelet level reduction in
different-aged populations. A possible improvement in clinical
outcome could be observed with longer follow-up periods as left
ventricular systolic function was improved.
Conclusion
IC tirofiban improved coronary blood flow and myocardial
tissue perfusion effectively in diabetic STEMI patients during
primary PCI. Improved LVEF was also observed 30 days post
primary PCI. However, bleeding events and MACE rates showed
no significant difference between the groups.
References
1.
FarhanS,HöchtlT,Kautzky-WillerA,WojtaJ,HuberK.Antithrombotic
therapy in patients with coronary artery disease and with type 2 diabetes
mellitus.
Wien Med Chenschr
2010;
160
: 30–38.
2.
Ergelen M, Uyarel H, Cicek G, Isik T, Osmonov D, Gunaydin ZY,
et
al
. Which is worst in patients undergoing primary angioplasty for acute
myocardial infarction? Hyperglycaemia? Diabetes mellitus? Or both?
Acta Cardiol
2010;
65
: 415–423.
3.
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B,
et
al
. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary inter-
vention: a report of the American College of Cardiology Foundation/
American Heart Association task force on practice guidelines and the
society for cardiovascular angiography and interventions.
Circulation
2011;
124
(23): 574–651.
4.
Simes RJ, Topol EJ, Holmes DR Jr, White HD, Rutsch WR, Vahanian
A,
et al.
Link between the angiographic sub study and mortal-
ity outcomes in a large randomized trial of myocardial reperfusion.
Importance of early and complete infarct artery reperfusion. GUSTO-I
investigators.
Circulation
1995;
91
: 1923–1928.
5.
Brener SJ, Mehran R, Dressler O, Cristea E, Stone GW. Diabetes
mellitus, myocardial reperfusion, and outcome in patients with acute
ST-elevation myocardial infarction treated with primary angioplasty
(from HORIZONS AMI).
Am J Cardiol
2012;
109
: 1111–1116.
6.
Talarico GP, Brancati M, Burzotta F, Porto I, Trani C, De Vita M,
et
al.
Glycoprotein IIB/IIIA inhibitor to reduce postpercutaneous coro-
nary intervention myonecrosis and improve coronary flow in diabet-
ics: the ‘OPTIMIZE-IT’ pilot randomized study.
J Cardiovasc Med
(Hagerstown) 2009;
10
: 245–251.
7.
Wu TG, Zhao Q, Huang WG, Wei JR, Chen SW, Zhao J,
et al.
Effect of
intracoronary tirofiban in patients undergoing percutaneous coronary
intervention for acute coronary syndrome.
Circ J
2008;
72
: 1605–1609.
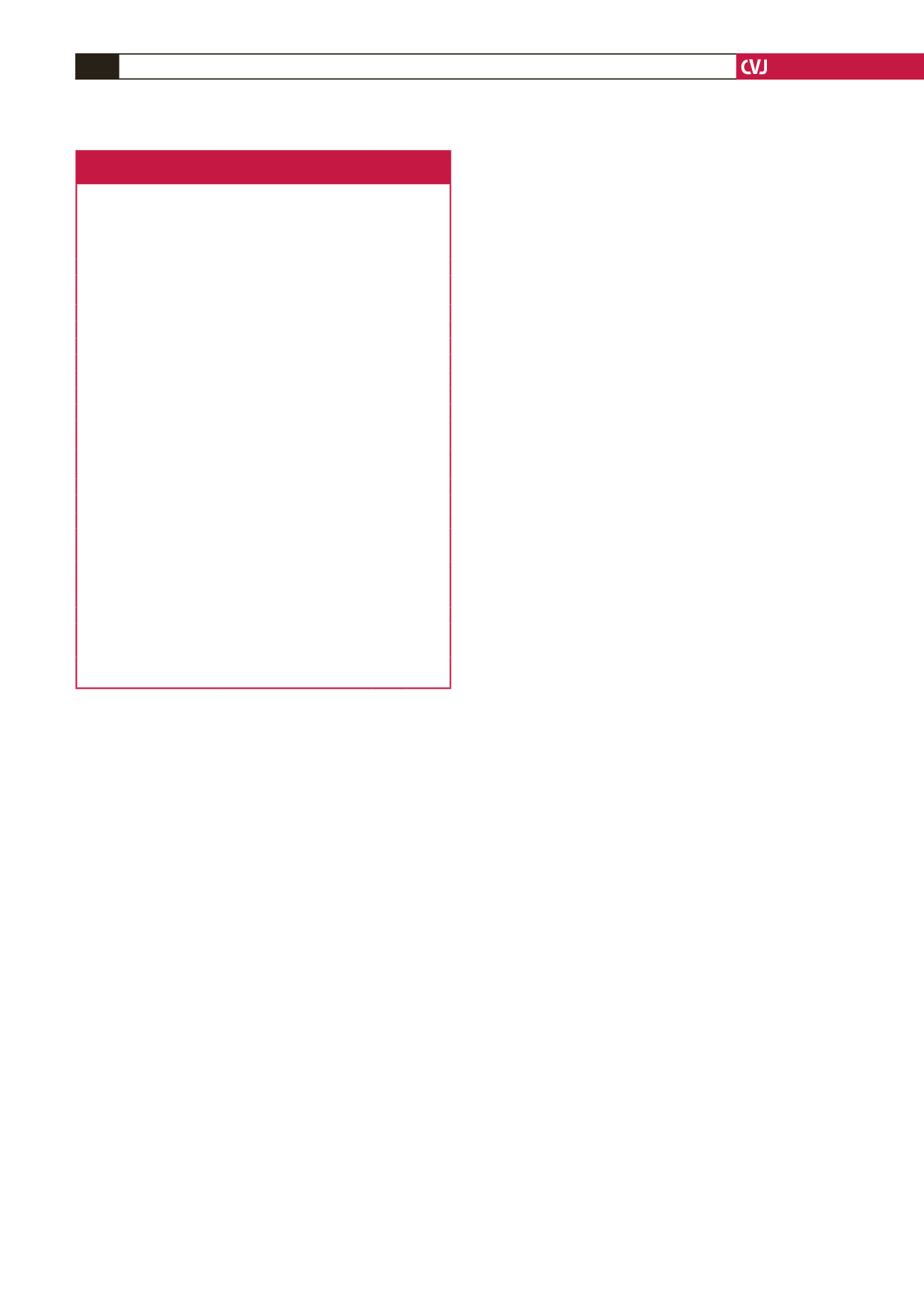
Table 3. Summary of angiographic characteristics,
MACE and bleeding events in both groups
Parameters
Group A (IV)
(
n
=
50)
Group B (IC)
(
n
=
45)
χ
2
/t
p-
value
TIMI 3 flow after procedure,
n
(%)
39 (78)
42 (93)
4.02 0.045*
MBG 3 after procedure
34 (68)
41 (82)
5.34 0.021*
Infarct-related vessel,
n
(%)
Left anterior descending
artery,
n
(%)
30 (60)
25 (55)
0.38 0.72
Circumflex artery,
n
(%)
7 (14)
5 (11.1)
0.072 0.91
Right coronary artery,
n
(%)
10 (20)
13 (28.8)
0.065 0.92
Triple vessels,
n
(%)
3 (6)
2 (4.4)
0.00 1.00
Balloon,
n
(%)
10 (20)
13 (28.8)
0.98
In-hospital MACE,
n
(%)
In-hospital death,
n
(%)
2 (4)
1 (2.2)
0.00 1.00
In-hospital stroke,
n
(%)
0
0
0.00 1.00
In-hospital re-infarction,
n
(%)
1 (2)
0
0.05 0.993
In-hospital stent thrombo-
sis,
n
(%)
1 (2)
0
0.05 0.993
In-hospital TVR,
n
(%)
0
0
0.00 1.00
1-month MACE,
n
(%)
1-month death,
n
(%)
1 (2)
0
1.00
1-month stroke,
n
(%)
0
0
0.00 1.00
1-month re-infarction,
n
(%)
1 (2)
1 (2.2)
0.00 1.00
1-month stent thrombosis,
n
(%)
1 (2)
1 (2.2)
0.00 1.00
1-month TVR,
n
(%)
1 (2)
1 (2.2)
0.00 1.00
TIMI major bleeding,
n
(%)
1 (2)
1 (2.2)
0.00 1.00
TIMI minor bleeding,
n
(%)
5 (10)
4 (8.8)
0.02 0.95
Thrombocytopenia,
n
(%)
2 (4)
2 (4.4)
0.00 1.00
TIMI: thrombolysis in myocardial infarction; MBG: myocardial blush grade;
MACE: major adverse cardiac events; TVR: target vessel restenosis.



















