
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 5, September/October 2019
AFRICA
291
respectively. Cumulatively, these effects increase cardiac output
and systolic blood pressure.
In the lumbar region, the efferent sympathetic nerves enter the
kidneys via the renal arteries. They arborise alongside the renal
artery, running in the vasa vasorum and terminate in the efferent
glomerular arteriole (EGA), juxta-glomerular apparatus (JGA)
and renal tubules. JGA activation results in renin release, which
activates the renin–angiotensin–aldosterone system (RAAS).
End-products of RAAS activation, angiotensin II (AT-II) and
aldosterone induce vasoconstriction and tubular sodium and
water retention, respectively. AT-II constricts the EGA, which
raises intra-glomerular pressure and filtration rate. AT-II also
increases peripheral resistance, which increases diastolic blood
pressure, cardiac afterload and coronary perfusion.
It is almost incomprehensible that mere stretching of the
renal pelvis by increased urine production would produce
such a cascade of events that result in increased cardiac
output, augmented glomerular filtration and subsequent adrenal
activation. The primary renal aim would be to restore water and
sodium balance acutely. Chronic and inappropriate activation
of this system results in hypertension and its sequelae. Although
IST is not the only cause of essential hypertension, there is strong
evidence that the autonomic nervous system plays a critical role
in hypertension pathogenesis and endothelial health.
10,11
Hypertensive heart disease and cardiac arrhythmia
Uncontrolled hypertension often results in hypertensive heart
disease (HTHD), which provides an ideal arrhythmic substrate.
12
Interstitial cardiac fibrosis, promoted by aldosterone secretion,
fractionates the depolarising electrical wave front. Left ventricular
hypertrophy (LVH) associates with increased myocardial oxygen
consumption, and in the presence of concomitant coronary
atherosclerosis, the endocardium remains at an increased risk
of hypo-perfusion and myocardial death. Often, coronary
plaques rupture because of a sudden surge in blood pressure
or increased intra-plaque inflammation. IST has been shown to
associate with both precipitants.
13
Additionally, in patients with
obstructive sleep apnoea, sympathetic surges followed by intense
vagal reflexes have been shown to precipitate paroxysmal atrial
fibrillation (AF) and associate with nocturnal SCD.
14
Renal denervation to modulate autonomic
activity: human proof-of-principle studies
The hypothesis that denervation of the renal sympathetic nerves
should result in blood pressure reduction was successfully
tested in clinical trials. In humans, non-selective surgical
splanchnicectomy, which includes RD, was frequently performed
as primary hypertension (HT) treatment,
15
but common
side effects, such as impotence, orthostatic hypotension and
incontinence, led to its disappearance from current-day practice.
This led to the concept that the efferent nerves in the renal artery
adventitia might yield an easily accessible target. The advent of
endovascular therapy made access to the renal arteries possible
through femoral artery puncture (Fig. 2). Heradien
et al
. recently
reported that RD could also be performed via brachial or radial
artery puncture.
16
This unique form of RD vascular access
eliminates the risk of groin-related hypertensive arterial bleeding
and allows same-day hospital discharge.
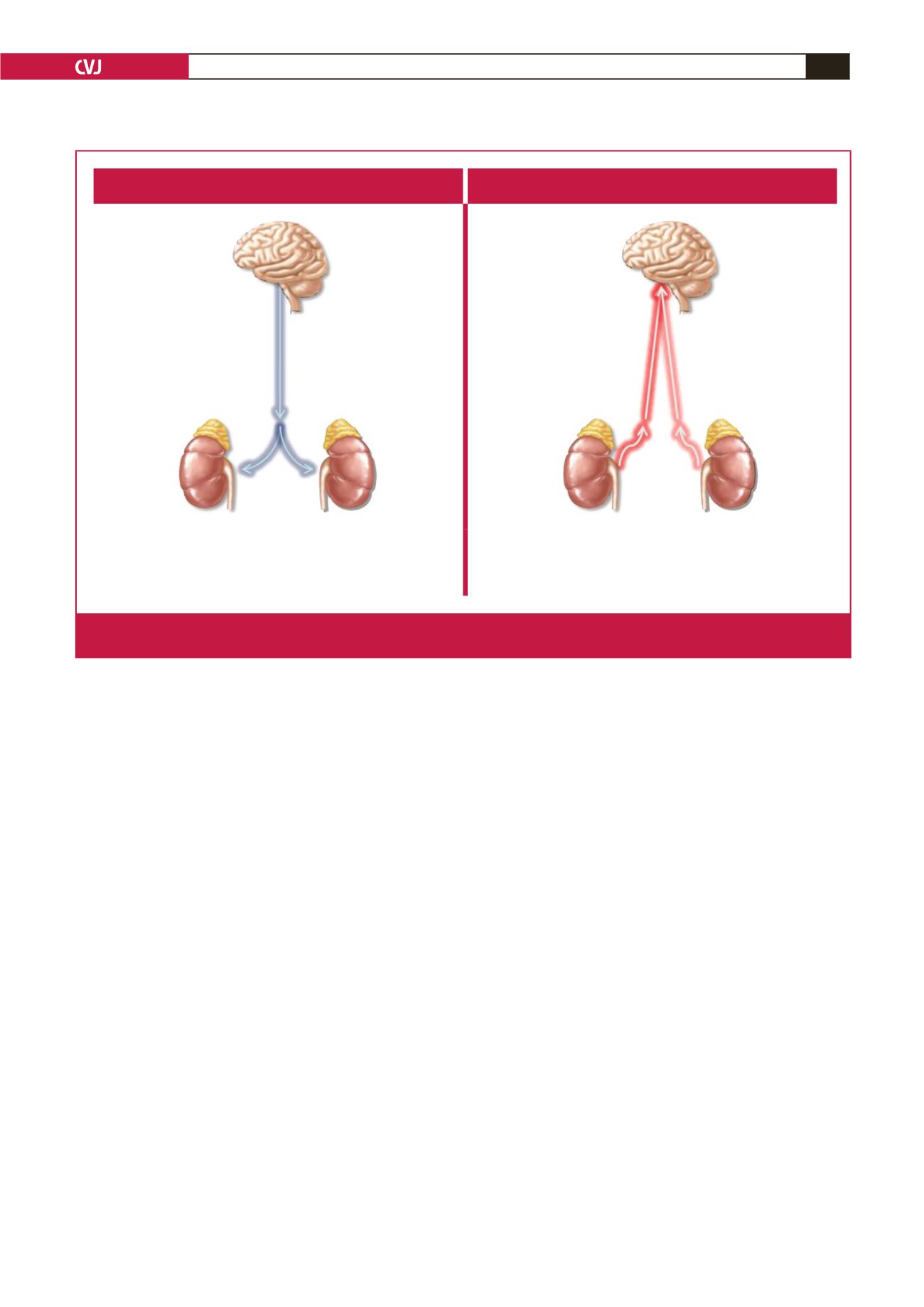
Efferent sympathetics
Afferent renal sympathetics
• Renin release – RAAS
• Na absorption
• Renal blood flow (TPR)
• The kidney is a source of central sympathetic activity,
sending signals to the CNS
Fig. 1.
Renal sympathetic nerves facilitate brain–kidney cross-talk and play a central role in BP control and regulation of autonomic
tone (supplied by Medtronic, Inc).



















