
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 5, September/October 2019
292
AFRICA
Landmark RD trials
The landmark endovascular RD trials are often colloquially
referred to as the Symplicity HTN Trilogy. The first trial that
kindled interest was published a decade ago. SYMPLICITY
HTN-1 was a multicentre, non-randomised, safety and proof-
of-principle cohort study.
17
Patients with so-called resistant
HT, defined as an office blood pressure (BP)
≥
160/90 mmHg
on three drugs, including a diuretic, underwent bilateral RD.
17
Compared to baseline, follow-up office BP was dramatically
reduced and the scientific world was sensitised that RD might
offer a potential cure for the proverbial ‘silent killer’.
18
SYMPLICITY HTN-2 was the first randomised, controlled
trial (RCT) that tested the hypothesis that RD was superior to
medical therapy in the management of resistant HT.
19
Again,
similarly to SYMPLICITY HTN-1, office systolic BP was
reduced with RD by 32 mmHg at the six-month follow up.
This trial resulted in an all-time high interest and a flickering
hope that RD might add an important new weapon in the fight
against HT. Whereas the procedure was registered for use in
European countries, the Food and Drug Administration insisted
on a further trial before registration in the USA; hence, the
SYMPLICITY HTN-3 trial was designed.
20
SYMPLICITY HTN-3 randomised 535 treatment-resistant
hypertensive patients to RD or sham RD. The results were
interesting but unexpectedly disappointing. Although both
groups had significant office BP reductions at the six-month
follow up, RD did not meet the primary efficacy endpoint of the
mean difference between groups of 5-mmHg reduction in office
systolic blood pressure (SBP). These surprising results brought
the ‘speeding RD train to a grinding halt’.
21
However, several
confounders have been identified that may have contributed to
the failure of SYMPLICITY HTN-3.
22
Despite rigorous trial design and execution, several
unaccounted for factors may have contributed to the failure
of SYMPLICITY HTN-3 to demonstrate RD efficacy relative
to the sham control.
23
These include patient demographics,
medication adherence, the Hawthorne effect, the placebo effect,
trial conduct, regression to the mean, operator experience and
catheter design.
Patient demographics:
Unlike previous SYMPLICITY trials,
SYMPLICITY HTN-3 also recruited African-American (AA)
patients (26% of the prospective cohort). Compared to the
non-AA sub-group, AA patients in the sham group had a
9.2-mmHg greater decline in office SBP at six months. This
change in sham office SBP was nearly twice as large in AA as
non-AA patients. In a
post hoc
analysis, the authors concluded
that this unexpected BP reduction in a sham group was likely due
to increased post-randomisation medication adherence and that
the change after renal denervation was probably not confounded
by race.
24
Although this exploratory report does not provide definitive
evidence that the SBP response to RD differed by race, it is
generally accepted that hypertensive patients of African ancestry
are poor responders to angiotensin converting enzyme (ACE)
inhibitor and beta-blocker therapy.
25
This dogma was recently
challenged in the Creole study where investigators found that
black Africans responded better to perindopril–amlodipine than
to perindopril–thiazide combination therapy.
26
Despite these
encouraging results that black Africans may respond to ACE
inhibitor therapy, it remains to be proven that blacks are poor
RD responders.
In the current South African environment, however, racial
confounding in science led to the retraction of a controversial
article that was recently published.
27
Unfortunate events like
these may hamper expedient ethical approval of BP studies
investigating different racial responses to antihypertensive
treatment.
Many have hypothesised that the beneficial effects of RD
may be attenuated in patients with later-stage peripheral
artery disease or increased vascular stiffness, which might limit
the capacity for reverse vascular remodelling following the
procedure. Indeed, several reports indicate that various indices
of increased arterial stiffness predict improved BP response
following RD.
28-31
Likewise, Mahfoud and colleagues showed in
two separate retrospective analyses that patients with isolated
systolic hypertension, a course but easily determined identifier
of increased arterial stiffness (defined as office SBP
>
140 mmHg
and DBP
<
90 mmHg), had more significant BP drops than
patients with combined systolic and diastolic hypertension.
32
For this reason, patients with isolated systolic hypertension were
explicitly excluded from the sham controlled RCTs that followed
SYMPLICITY HTN-3.
Medication adherence:
Although patients were encouraged to
continue taking their prescribedmedication diligently throughout
follow up, urine or blood levels of antihypertensive drugs were
not measured. Surprisingly, about 40% of the patients changed
their antihypertensive medication regime after randomisation.
Furthermore, recent evidence from multiple hypertension trials,
including RDN trials, clearly indicates that non-adherence to
prescribed medications is common, perhaps greater than 50%,
and may vary within patients even during the clinical trial follow-
up period.
33
Such rampant non-adherence may be due to multiple factors,
including lack of understanding of the risks and benefits
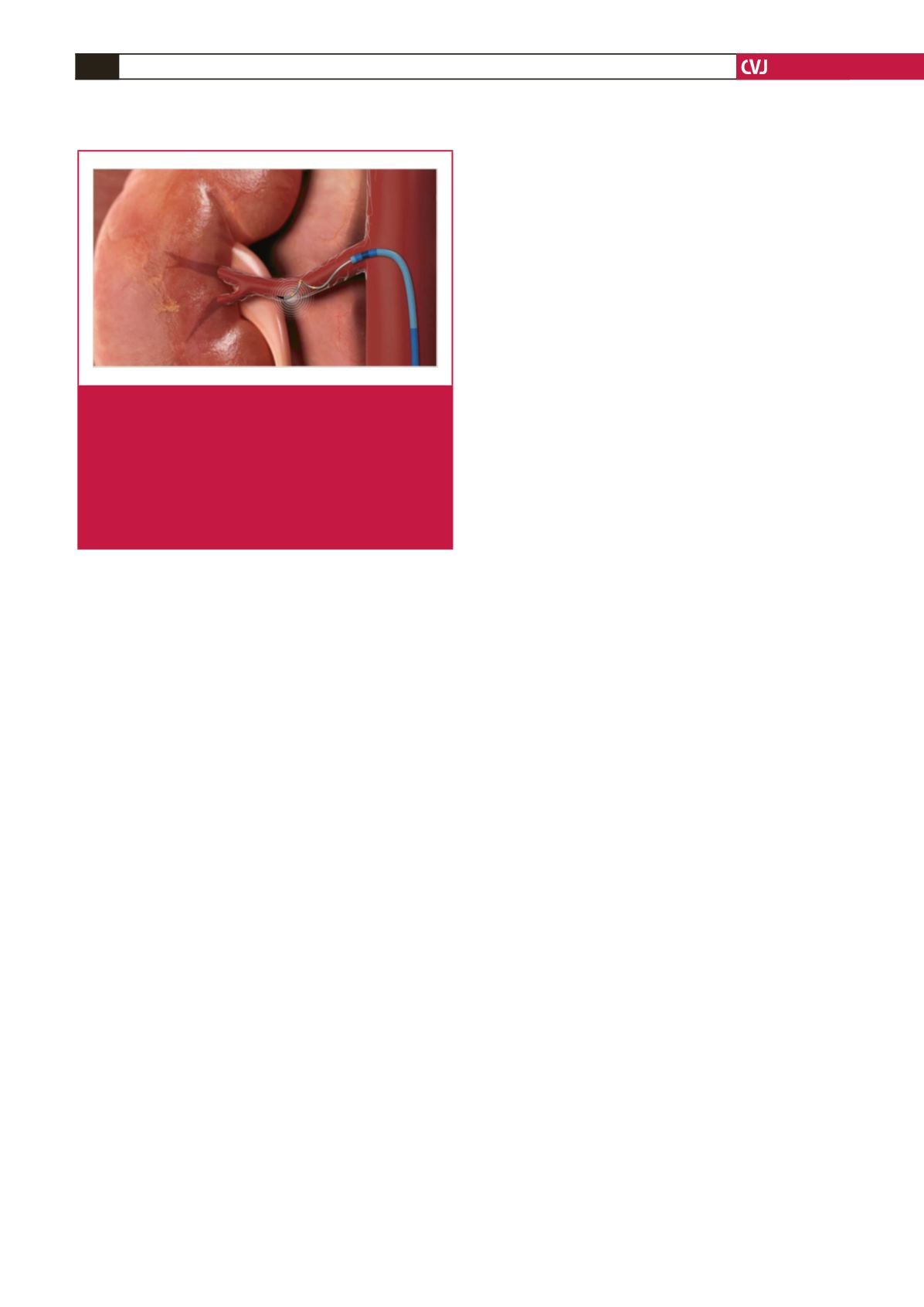
Fig. 2.
Renal denervation is accomplished with a quadripolar
radiofrequency catheter via arterial puncture. The
catheter is advanced over a guidewire into the distal
renal artery, the wire is removed and the catheter
conforms in a spiral form to make close contact with
the vessel wall. Radiofrequency heat energy is then
delivered in an attempt to destroy the efferent renal
nerves in the vasa vasorum (copyright for figure
obtained from Medtronic, Inc).



















