
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 4, July/August 2020
170
AFRICA
Autophagy is a dynamic process beginning with the induction
of autophagosome formation and ending with its degradation
in lysosomes.
12-14
Evaluation of flux can be done experimentally
through lysosomal blockade, or indirectly, inferred from changes
in the expression of p62/SQSTM1. Chloroquine has routinely
been used for evaluation of autophagic flux: the drug disrupts
autophagy by inhibiting the acidification of lysosomes that fuse
with the autophagosomes and thereby rescues p62/SQSTM1
breakdown,
15,16
indicating flux rather than steady-state levels.
Therefore it was advised that Western blots should be paired with
the same measurement in the presence of lysosomal blockade
with chloroquine or bafilomycin A.
12
However, little is known
about the effects of chloroquine
per se
on the mitochondrial
mitophagy process in myocardial ischaemia/reperfusion.
As far as we are aware, the temporal relationship between
changes in mitochondrial oxidative phosphorylation function
and mitophagy during exposure of the heart to ischaemia/
reperfusion injury is still largely unexplored. The aim of this
study was to gain more insight into the mitochondrial oxidative
phosphorylation processes as well as mitophagy in hearts of
rats at the end of an ischaemic episode and after a period
of reperfusion. To allow assessment of autophagic flux, an
additional series of experiments was performed in rats pre-treated
with chloroquine before subjecting the hearts to ischaemia/
reperfusion
ex vivo
.
Interpretation of the results obtained could be complicated
by the fact that chloroquine
per se
is known to have cardiotoxic
effects at both therapeutic and high doses, especially when
administered rapidly, including cardiovascular effects such as
vasodilation, hypotension, suppressed mechanical function and
cardiac arrhythmias.
17,18
These negative effects on myocardial
function could affect the response of the heart to ischaemia/
reperfusion and therefore the autophagy/mitophagy process.
To evaluate the use of chloroquine as indicator of mitophagic
flux in myocardial ischaemia/reperfusion, it was necessary to
establish its effects on myocardial function before induction of
ischaemia/reperfusion. In this study, rats were therefore treated
with a low dose of chloroquine before experimentation and its
effects were assessed on myocardial as well as mitochondrial
function and mitophagy in a well-characterised
ex vivo
model
of ischaemia/reperfusion. Such an approach would allow
evaluation of chloroquine effects on myocardial as well as
mitochondrial function and mitophagy after exposure of the
heart to ischaemia/reperfusion.
Methods
Male Wistar rats weighing 230
±
10 g were used for this study.
They had free access to food and water and were kept on a
12-hour day/night cycle in the Central Research Facility of the
Faculty of Health Sciences of the University of Stellenbosch.
This study was approved by the Committee for Ethical Animal
Research of the Faculty of Health Sciences, University of
Stellenbosch. The study conformed to the revised South African
National Standard for the Care and Use of Animals for
Scientific Purposes (South African Bureau of Standards, SANS
10386, 2008).
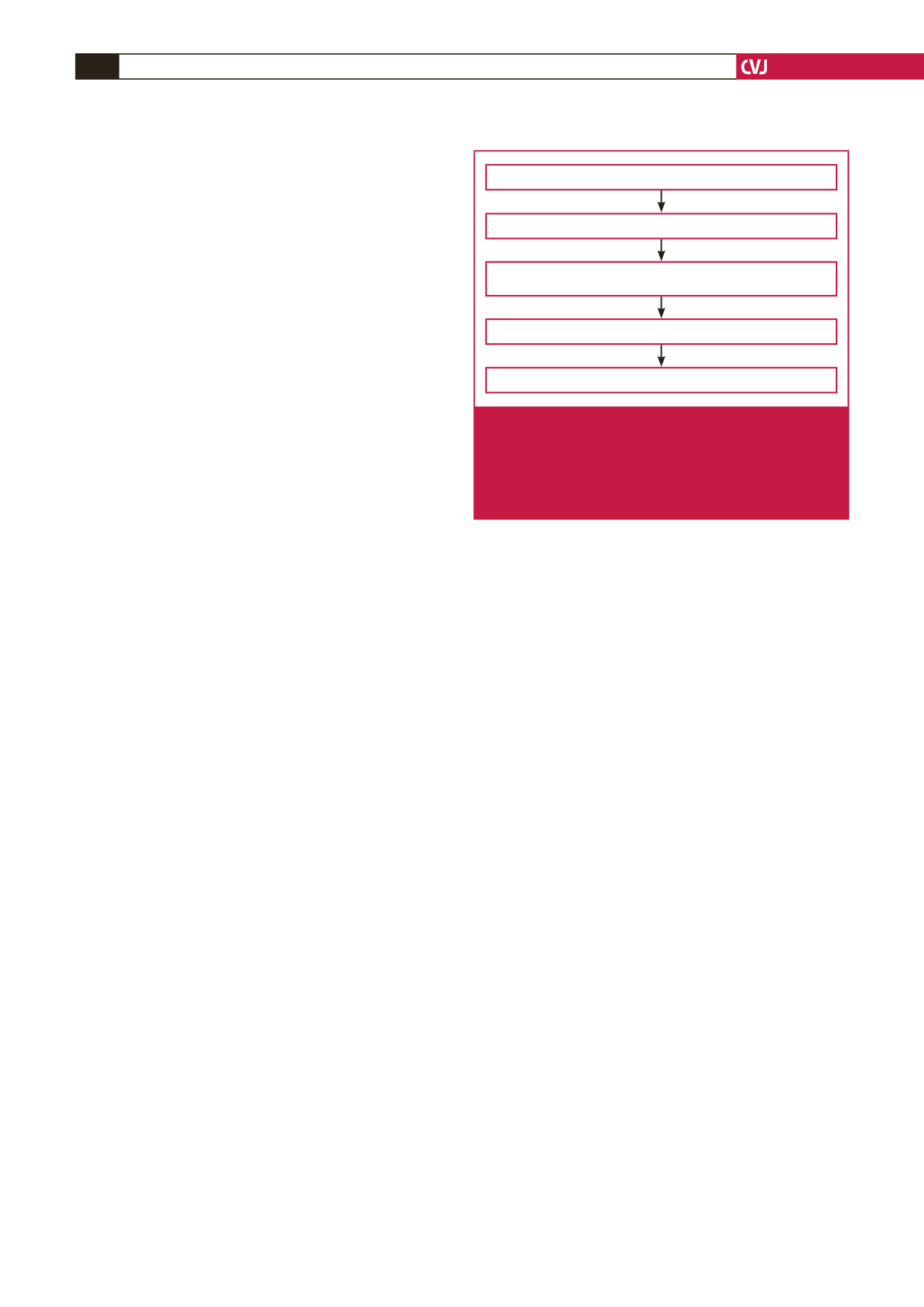
The experimental protocol followed is summarised in Fig.
1. Rats were divided into two groups, an untreated control
and a chloroquine-treated group. One hour before initiation
of experimentation, the rats were weighed and the latter group
was treated with chloroquine (10 mg/kg, intraperitoneally). The
control untreated rats received an equal volume of distilled
water, intraperitoneally. Chloroquine was freshly prepared every
day (10 mg/ml distilled H
2
O). Rats were anaesthetised by
intraperitoneal injection of sodium pentobarbitone (160 mg/kg).
After removal, the hearts were perfused as described below for
subsequent preparation of mitochondria
.
The hearts were perfused with modified Krebs-Henseleit
bicarbonate buffer (KHB) containing (in mM): NaCl 119,
NaHCO
3
24.9, KCl 4.7, KH
2
PO
4
1.2, MgSO
4
.7H
2
O 0.59, Na
2
SO
4
0.59, CaCl
2
.H
2
O 1.25 and glucose 10. KHB was oxygenated and
kept at pH 7.4 by gassing with 95% O
2
/5% CO
2
at 37°C. After
removal, the hearts were arrested in ice-cold saline, mounted
onto the aortic cannula and the left atrium was cannulated via
the pulmonary vein.
Hearts were then stabilised for 40 minutes [10 minutes
retrograde, followed by 20 minutes working mode (preload 15
cm H
2
O, afterload 100 cm H
2
O) and 10 minutes retrograde
perfusion]. Perfused hearts were allowed to beat spontaneously
and peak systolic pressure was recorded using a Statham
pressure transducer (Transpac IV, Abbotts, Sligo, Ireland), which
was inserted in the aortic cannula. Pressure signals were recorded
in 10-second pulses and analysed using software developed by
the University of Stellenbosch Electronic Department.
After stabilisation, hearts were subjected to 25 or 30 minutes
of global ischaemia, followed by 10 minutes of reperfusion.
Myocardial temperature was thermostatically controlled by
inserting a temperature probe into the pulmonary artery. The
temperature was monitored at regular intervals and kept at
36.5°C during ischaemia
.
Measurements of function were heart
rate (beats per min), aortic output (AO) (ml/min), cardiac
output (CO: coronary flow + aortic output) (ml/min), aortic
pressure (P
AO
) and work total (mW). Work total was calculated
as described by Kannengieser
et al
:
19
Work total = 0.00222(P
AO
– 11.25)(CO)
For isolation of subsarcolemmal mitochondria, at the end of
the stabilisation, ischaemic or reperfusion periods as described
Preparation of mitochondria (divide each pellet into two parts)
Injection with chloroquine or water 1 h prior to experimentation
Anaesthesia & removal of hearts
Perfusion: 40 min stabilisation, 25 min global ischaemia,
10 min reperfusion
40 min stabilisation, 30 min global ischaemia, 10 min reperfusion
Fig. 1.
Experimental protocol. Mitochondria were prepared
after 40 minutes of stabilisation; after 25 minutes of
global ischaemia; after 10 minutes of reperfusion
following 25 minutes of global ischaemia; after 30
minutes of global ischaemia; after 10 minutes of reper-
fusion following 30 minutes of global ischaemia.



















