
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 3, May/June 2021
136
AFRICA
pressure correlated inversely with CRAE, while triglycerides
correlated positively with CRVE. None of the cardiometabolic
variables correlated with AVR. Furthermore, correlation analyses
failed to show a relationship between FMD% and the retinal
microvascular calibres (not shown). Participants in whom retinal
tortuosity was positively identified, had significantly higher
diastolic blood pressure values compared to those without
retinal tortuosity [data expressed as mean (95% CI): tortuosity
present: 85.4 (80.2–90.6) mmHg vs tortuosity absent: 78.3
(76–80.5) mmHg;
p
=
0.01].
Relationships between cardiovascular risk factors and vascular
variables were tested with ANCOVA (all models adjusted for age).
Overweight or obese participants (BMI
≥
25 kg/m
2
) had significantly
higher FMD% compared to normal-weight counterparts [data
expressed as mean log FMD% (95% CI): overweight: 1.1 (0.9–1.3)
vs normal weight: 0.9 (0.8–0.9);
p
=
0.03]; however the significance
disappeared when the model was additionally adjusted for gender.
Similarly, participants with high total cholesterol levels (
>
5.1
mmol/l) presented with increased FMD% compared to those with
normal cholesterol values [mean log FMD% (95 CI): high total
cholesterol: 1.2 (0.9–1.5) vs normal total cholesterol: 0.9 (0.8–0.9);
p
=
0.03], but the significance was lost when additionally adjusting
for gender. No other cardiovascular risk factors were associated
with changes in FMD%.
The presence of systolic hypertension (systolic blood pressure
≥
140 mmHg) was associated with significantly decreased CRAE
(Fig. 2A), which was not affected by additional adjustment
for gender, however, the significance was lost when CRVE was
added as an adjustor (not shown). CRVE was significantly
lower in participants with systolic hypertension (Fig. 2B), even
when additionally adjusting for gender, however, the significance
disappeared after including CRAE as a covariate in the model
(not shown).
Diastolic hypertension (diastolic blood pressure
≥
90 mmHg)
was associated with significantly decreased CRVE, and although
significance was not affected when additionally adjusting for
gender, the inclusion of CRAE in the model moderated the
significance level to
p
=
0.057 (not shown). There were no
associations observed between any of the cardiovascular risk
factors and AVR.
Discussion
Evidence emanating from both official statistical sources and
100
90
80
70
60
50
40
30
20
10
0
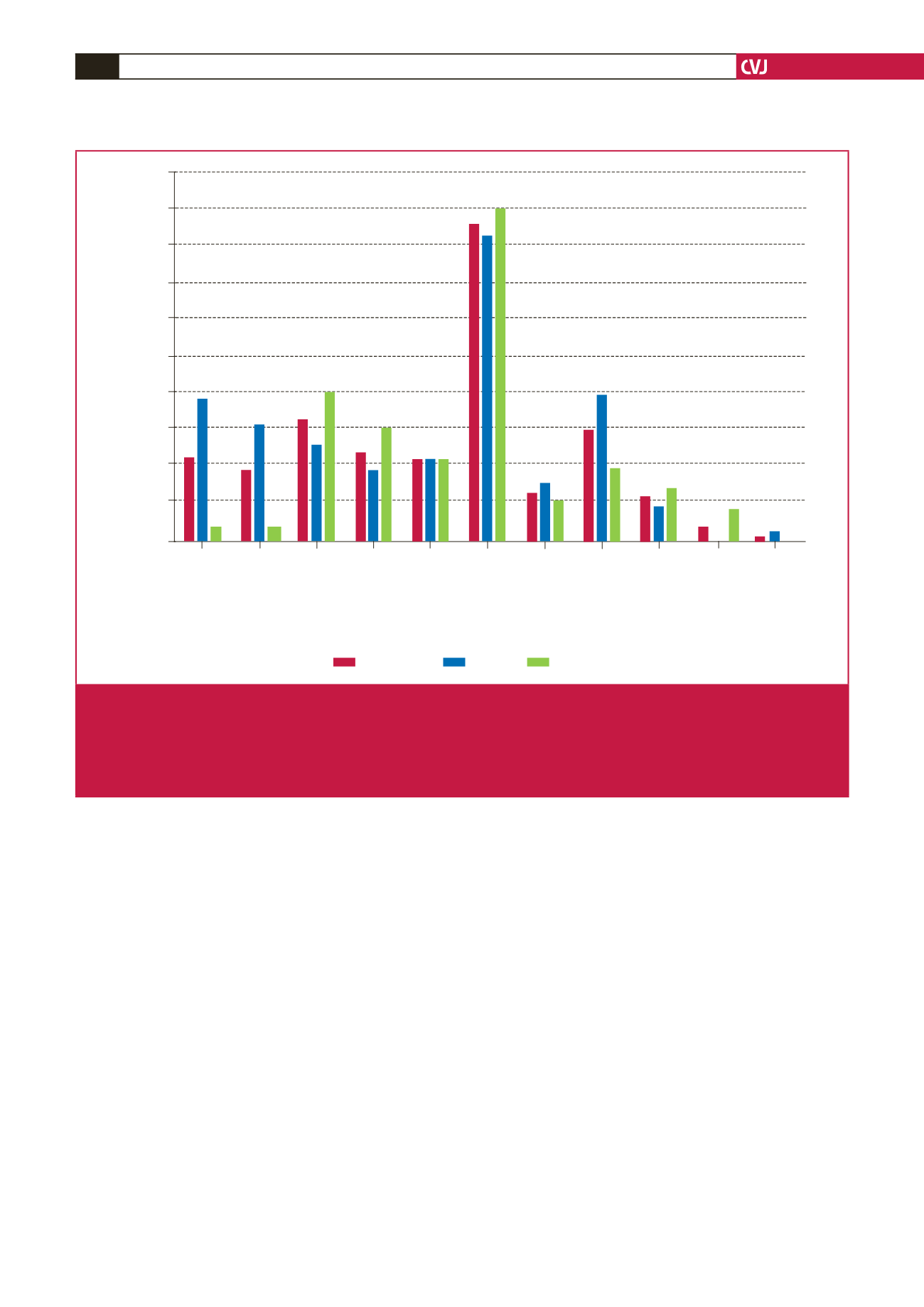
Relative frequency (%)
Overweight/obese
Central obesity
Systotic hypertesion
Diastolic hypertension
Smoker (current)
High total cholesterol
Low HDL cholesterol
High LDL cholesterol
High triglycerides
High fasting glucose
High fasting HbA
1c
Whole cohort
Females
Males
*
*
*
Fig. 1.
Relative frequency of cardiovascular risk factors in the whole cohort, and in female and male subsets. Overweight/obese:
BMI
≥
25 kg/m
2
; central obesity: waist circumference
≥
94 cm for males and
≥
80 cm for females; systolic hypertension:
≥
140
mmHg; diastolic hypertension:
≥
90 mmHg; high total cholesterol:
>
5.1 mmol/l; low HDL-C:
<
1 mmol/l for males and
<
1.2 mmol/l
for females; high LDL-C:
>
3 mmol/l; high triglycerides:
≥
1.7 mmol/l; high fasting glucose:
≥
7 mmol/l; high HbA
1c
:
≥
6.5%. Cut-off
values for the cardiovascular risk factors are from previously published guidelines adapted from the European and International
Societies for Hypertension and the International Diabetes Foundation.
30,31
*
p
<
0.05 females vs males.



















