
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 3, May/June 2021
AFRICA
137
researchstudiesispointingtoahighprevalenceof cardiometabolic
diseases and risk factors in Cape Town and the Western Cape
Province of South Africa,
3-6
supporting global trends that
low- to middle-income countries carry a high cardiovascular
disease burden. The present study collected data from volunteer
participants recruited at the Uitsig health clinic, which serves
a predominantly low socio-economic status (SES) community
outside Cape Town. In recent years, research has increasingly
uncovered a link between SES and cardiovascular health, with
low-SES individuals being at a greater cardiovascular risk.
32
Detecting early markers of CVD is critical in the management
of the disease burden in high cardiovascular risk populations.
The assessment of vascular changes can be particularly useful in
this regard, with FMD previously being shown to be a marker
of future cardiovascular events,
11,12,14
and the quantitative analysis
of retinal microvasculature linked to the development of CVD.
33
Both these non-invasive vascular assessment techniques are new
to clinical research in South Africa.
In summary, the results of the present study, conducted
in a relatively young adult population with a high smoking
prevalence, show that the FMD% and CRAE values were
in line with those previously reported in other populations,
whereas comparisons of the CRVE values with those from
other studies were more varied. Furthermore, as previously
shown by others, female participants had increased FMD% and
decreased baseline brachial artery diameters compared to their
male counterparts. With the exception of modest relationships
with waist circumference and elevated BMI, FMD% showed no
association with any of the measured cardiometabolic variables.
The retinal microvascular calibres in our study cohort were
associated with blood pressure, which is in keeping with findings
from previous studies, and the presence of retinal tortuosity was
associated with increased diastolic blood pressure. There was
no relationship between FMD% and the retinal microvascular
calibres in this cohort.
Although no internationally standardised cut-off values exist
for FMD, the median FMD% recorded in the present cohort
Table 2. Correlations between cardiometabolic and vascular variables
in the cohort (
n
=
66)
Variables
FMD% CRAE CRVE
AVR
BMI
r
0.24
0.04
0.04
0.005
p
0.06
0.76
0.78
0.97
WC
r
0.27*
0.02
0.15
–0.11
p
0.04
0.84
0.24
0.39
WHR
r
0.02
–0.04
0.2
–0.22
p
0.87
0.74
0.12
0.09
Systolic BP
r
0.09
–0.35*
–0.23
–0.16
p
0.48
0.01
0.08
0.22
Diastolic BP
r
0.1
–0.26*
–0.2
–0.09
p
0.44
0.04
0.13
0.5
Total C
r
0.12
0.02
0.02
0.007
p
0.34
0.85
0.86
0.95
HDL-C
r
–0.04
–0.01
–0.05
0.03
p
0.75
0.91
0.68
0.84
LDL-C
r
0.24
0.01
–0.03
0.04
p
0.06
0.92
0.83
0.72
Triglycerides
r
–0.21
0.18
0.28*
–0.07
p
0.1
0.16
0.02
0.58
Fasting glucose
r
–0.22
0.05
0.03
0.03
p
0.09
0.67
0.8
0.81
HbA
1c
r
0.08
0.15
0.17
0.02
p
0.55
0.23
0.19
0.88
The following variables with a skewed distribution were logarithmically trans-
formed: FMD%, BMI, waist circumference, total cholesterol, HDL-C, LDL-C,
triglycerides and fasting glucose.
BMI, body mass index; WC, waist circumference; WHR, waist-to-hip ratio;
BP, blood pressure; Total C, total cholesterol; HDL-C, high-density lipoprotein
cholesterol; LDL-C, low-density lipoprotein cholesterol; HbA
1c
, glycated haemo-
globin; FMD, flow-mediated dilatation; CRAE, central retinal arteriolar equiva-
lent; CRVE, central retinal venular equivalent; AVR, retinal arteriolar–venular
ratio;
r
, Pearson’s correlation coefficient;
p
,
p
-value. *Significant.
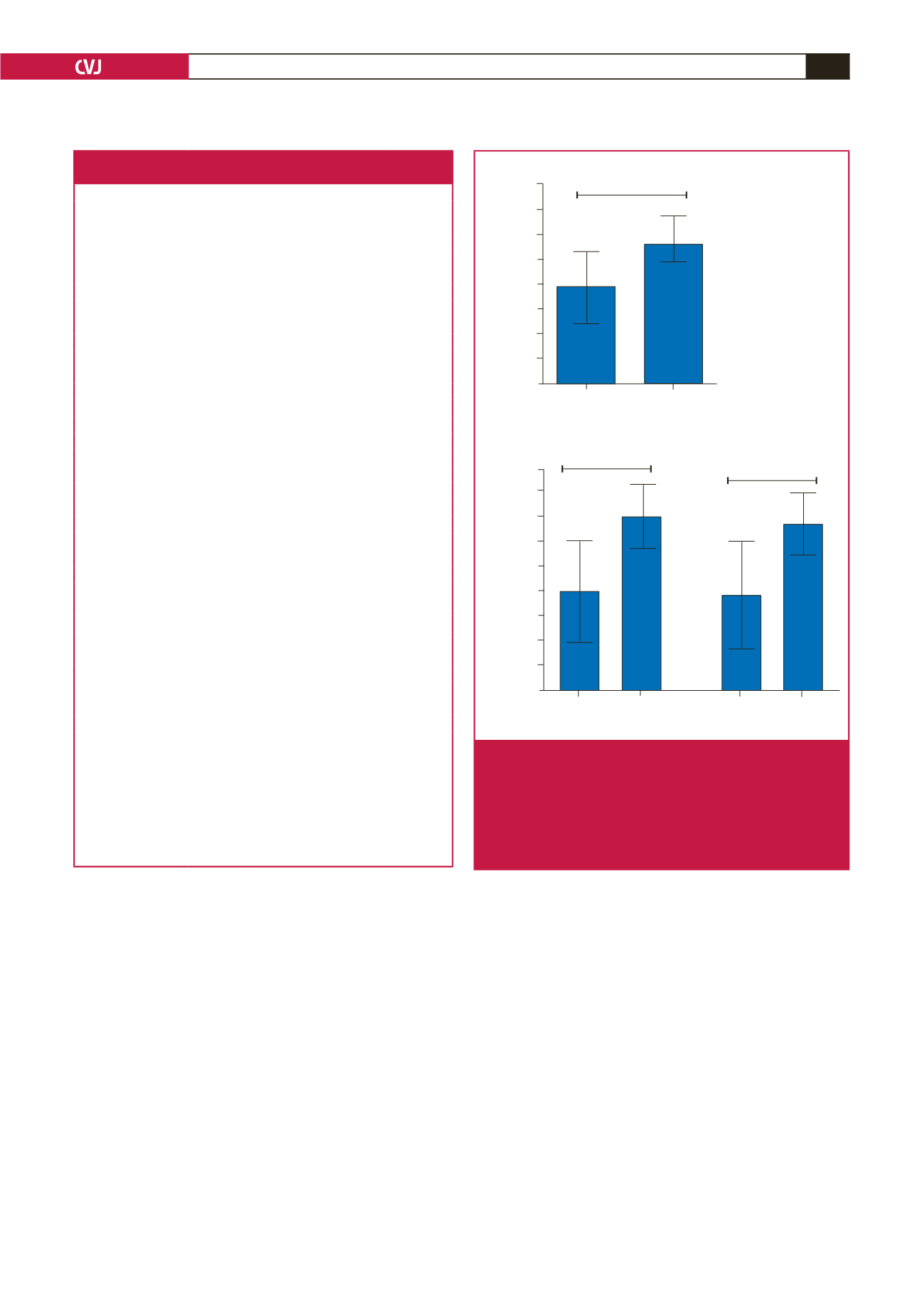
170
165
160
155
150
145
140
135
130
Yes
No
Systolic hypertension
*
#
#
265
260
255
250
245
240
235
230
225
220
Yes
No
Systolic hypertension
Yes
No
Diastolic hypertension
A
B
CRAE (
μ
m)
CRVA (
μ
m)
Fig. 2.
Relationships between cardiovascular risk factors and
retinal vascular variables. A. Effect of systolic hypertension
(systolic blood pressure
≥
140 mmHg) on CRAE; *
p
=
0.03.
B. Effects of systolic and diastolic hypertension (diastolic
blood pressure
≥
90 mmHg) on CRVE;
#
p
=
0.02. Data are
expressed as mean (95% CI); all ANCOVA models adjusted
for age.



















