CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 1, February 2012
AFRICA
45
prehypertension was reported, using PubMed, Ovid and the
Cochrane Library. Studies were identified using the keyword
‘prehypertension’. Further information was retrieved by a
manual search of references from recent reviews and relevant
published original studies. The reference lists of the articles
obtained were screened in order to identify other relevant refer-
ences, which were then retrieved.
We included cross-sectional studies that reported the preva-
lence of prehypertension among individuals over 15 years of
age. It had to be original research written in English and Chinese,
containing the minimum information necessary to conduct
pooled analysis of prevalence. There had to be a clear definition
of prehypertension according to the seventh annual report of the
Joint National Committee (JNC7): SBP between 120 and 139
mmHg or DBP between 80 and 89 mmHg.
Studies were excluded if the participants were limited to a
particular occupation (e.g. teachers) and population (e.g. chil-
dren or adolescence), or if there were multiple reports of the
same results. In addition, we excluded studies using non-JNC7
standards (e.g. normal/high-normal BP) to avoid inconsistency
of outcomes resulting from different blood pressure categories.
To avoid bias in the data abstraction process, two authors
independently collected the data from the articles and compared
results, with disagreements resolved by discussion among the
investigators. We extracted from the full-text articles the study
and population characteristics such as publication year, country
of data collection, characteristics of target population (e.g. base-
line age, gender and sample size), methods of blood pressure
measurement (e.g. mercury sphygmomanometer), prevalence
of prehypertension and quantitative data (i.e. raw numbers and
percentages) related to the meta-analysis.
Statistical analysis
We calculated crude prevalence and standard errors. Pooled
prevalence was estimated by Stata statistical software package
(version 11.0) using the command ‘metan’ with the use of a
random-effects model, which allows for heterogeneity of effects
between studies.
7
The heterogeneity among studies was tested by
Cochran’s
Q
test.
8
The quantity
I
2
that describes the percentage of
variation across studies included was calculated.
9,10
We conducted subgroup analyses to examine potential sourc-
es of heterogeneity according to: gender, region, sample size,
year of inception of the survey, and method of blood pressure
measurement. The mean age was excluded because this variable
was only available for half of the studies. We also tested the
heterogeneity by conducting a meta-regression analysis.
To study possible publication bias, we evaluated funnel plots.
A deficiency in the base of the funnel with asymmetry indicates
the presence of possible publication bias from unpublished small
studies. Publication bias was also assessed by two formal tests:
Begg’s adjusted-rank correlation test and Egger’s regression
asymmetry test. For all tests, a probability level less than 0.1 was
considered significant. All statistical analyses were performed
with Stata software 11.0.
Results
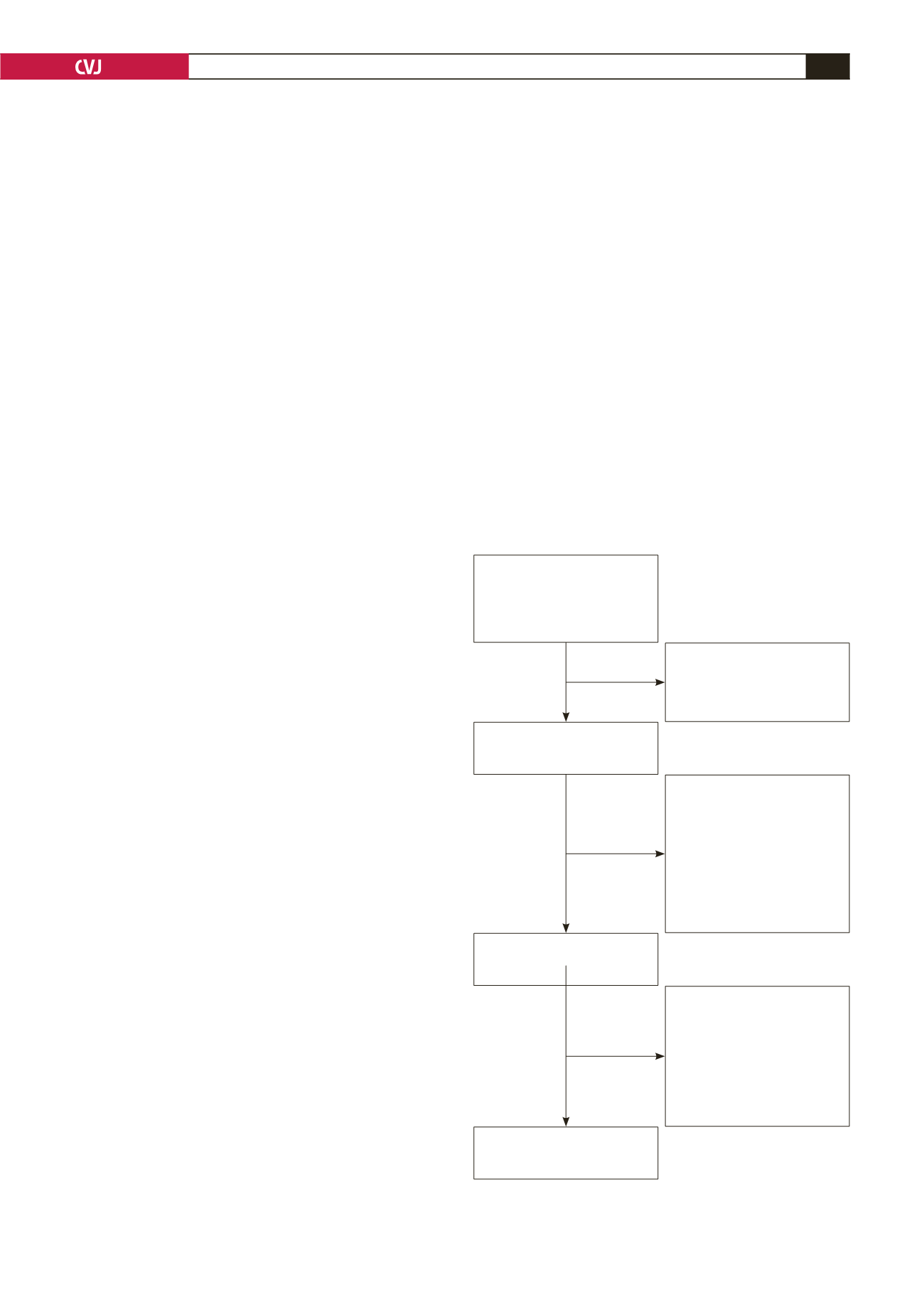
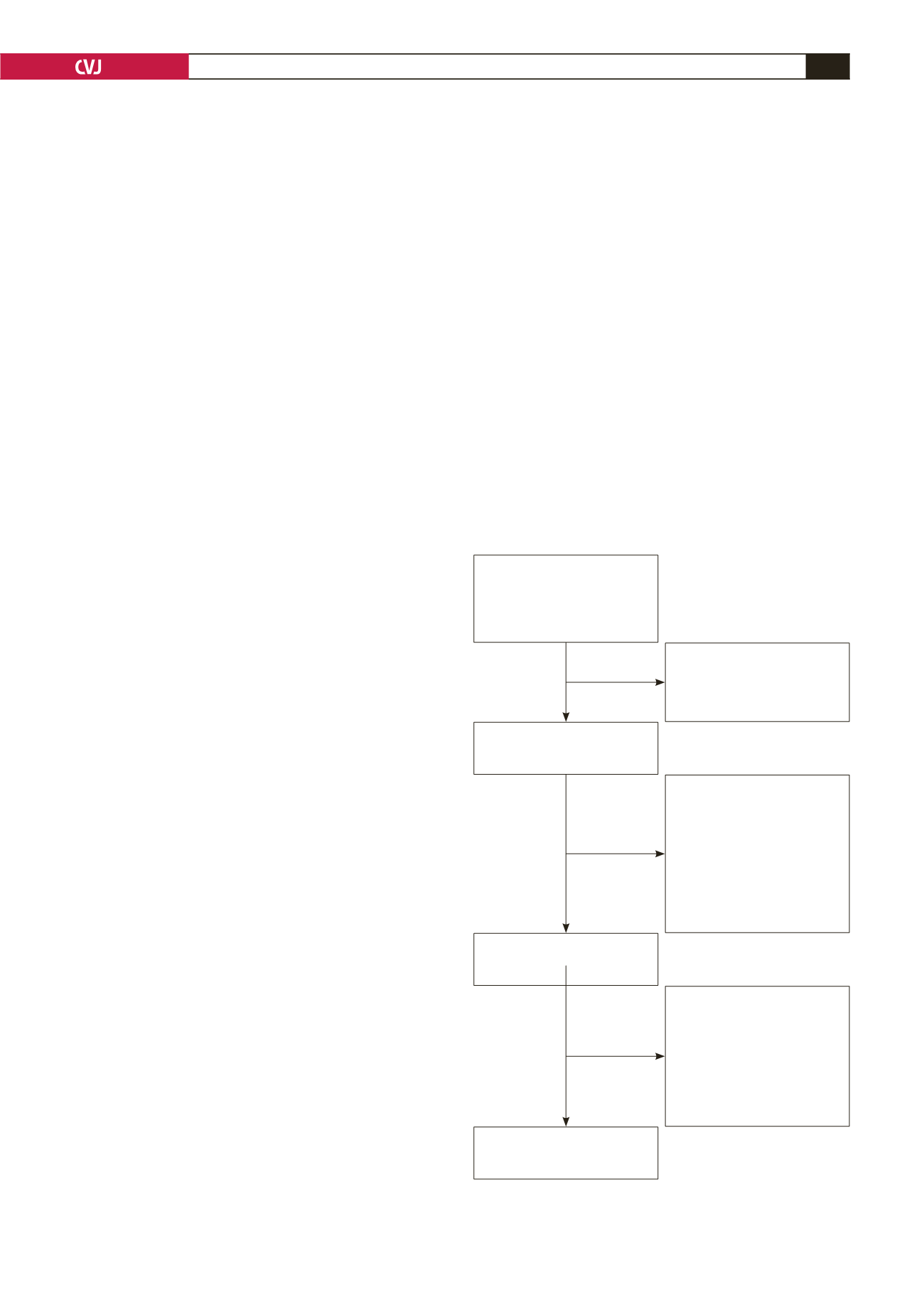
The literature searches yielded 1 923 articles. We assessed
abstracts and titles against the inclusion criteria, and selected 49
articles for a detailed examination. After reviewing the full texts,
a total of 22 studies
11-32
met our inclusion criteria. Fig. 1 shows
the selection process and reasons for excluding studies.
Our analysis included a total sample of 242 322 individuals
(126 899 females and 115 423 males). The studies included
were all published recently, the majority of which after 2005.
The sample sizes varied from 782 to 69 722 participants. Most
studies were distributed in Asia, including China, Japan, India,
Iran, Turkey and Korea. There were also studies from non-Asian
countries, such as the USA, Netherlands, Jamaica, Nigeria and
Ghana. Characteristics of studies included in the analyses are
described in Table 1.
Pooled results from the meta-analysis
The prevalence of prehypertension varied widely, from 14.5%
in the study by Erem
et al.
16
to 58.7% in the study by Isezuo
et
al.
20
Fig. 2 shows the overall estimates of prevalence and 95%
confidence intervals (CI) from the individual countries. Meta-
analysis of all 22 studies yielded an overall pooled prevalence of
38% (95% CI: 32–43%), with substantial heterogeneity observed
(
χ
2
=
14430.35,
p
=
0.000,
I
2
=
99.9%).
Titles and abstracts identified
(
n
=
1 923)
Pubmed (
n
=
1 119)
Ovid (
n
=
755)
Cochrane Library (
n
=
49)
Reasons for exclusion:
Not relevant, case reports,
reviews, editorials, or animal
studies.
Included:
Cross-sectional estimates of
prevalence
Original research written in
English and Chinese.
Contained the minimum
information necessary for
pooled analysis.
Use of JNC7 definition of
prehypertension
Excluded:
Non-JNC7 standard (
n
=
3)
Multiple reports of the same
result (
n
=
11)
Studies limited to a particular
population or occupation
(
n
=
9)
No original data (
n
=
1)
Other reasons (
n
=
3)
Abstracts retained for a
detailed assessment (
n
=
236)
Full-text studies examined in
detail (
n
=
49)
Studies included in meta-
analysis (
n
=
22)
Fig. 1. Flow chart showing the process of selection of the
relevant studies.