CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 1, February 2012
48
AFRICA
involved are complicated, including activation of the renin–
angiotensin system, the impact of progesterone and aldosterone,
leptin levels and the regulation of oestrogen.
38-42
The prevalence of prehypertension would be expected to be
higher among women after menopause, and the difference in
prevalence between older men and women may be less obvious.
We found in our analysis however that the prevalence of prehy-
pertension was higher among males than females (41 vs 34%).
Although a pooled analysis of different age groups was not
conducted due to insufficient data, we concluded that males are
generally more at risk for prehypertension than females.
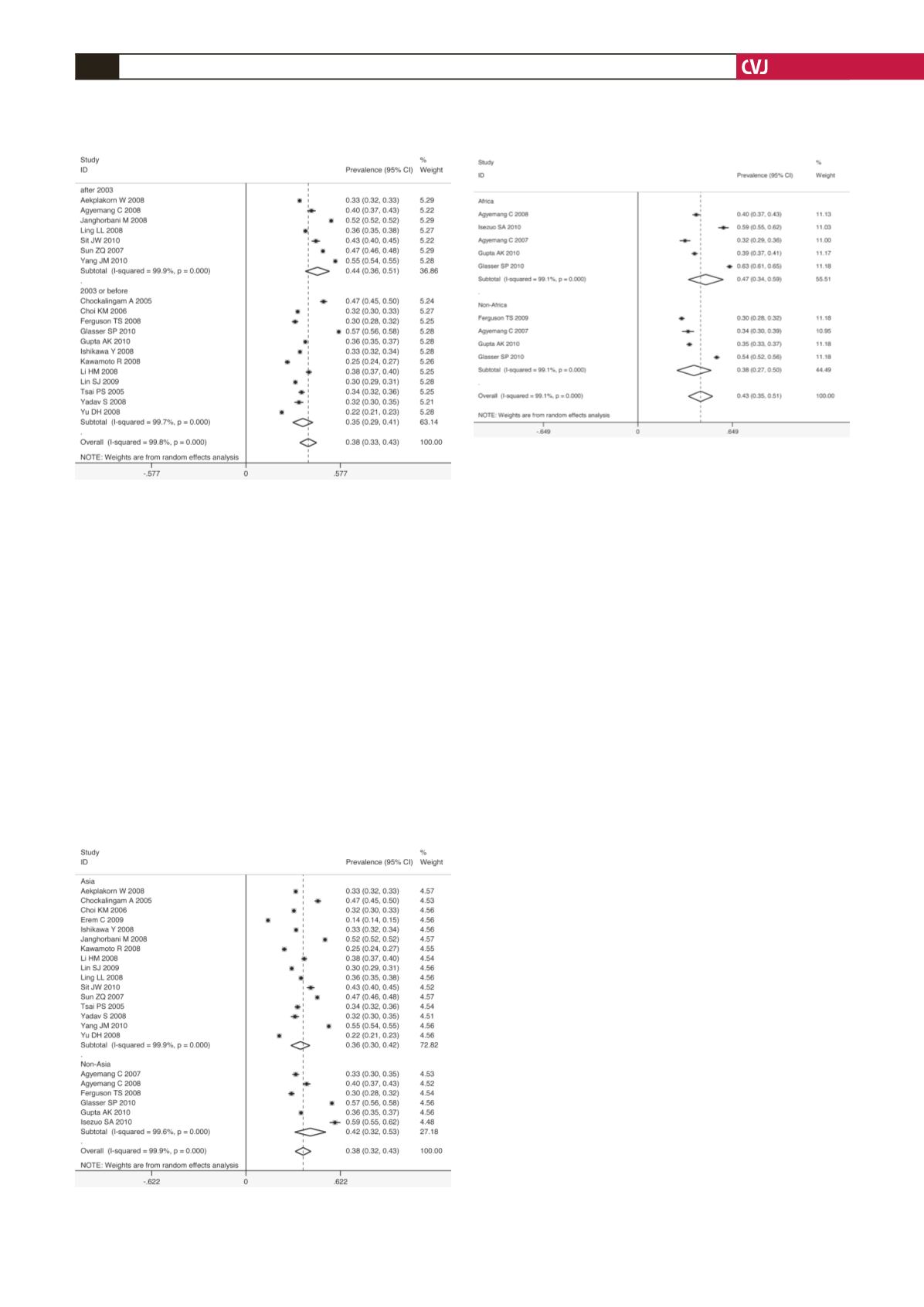
Within our expectation, a large variation in estimates of
prevalence of prehypertension was found. This variability was
not explained by gender ratio, sample size of the survey, region
of the study or method of blood pressure measurement. However,
some of these variables did change the estimated prevalence of
prehypertension.
The maximum and minimum prevalence rates of prehyper-
tension were observed in Nigeria and Turkey, respectively. The
pooled prevalence was higher among non-Asian individuals
(42%) than in the Asian population (36%). In the non-Asian
subgroup, a high prevalence of 47% was observed among the
African population, possibly due to ethnic diversity and differ-
ences in lifestyle.
The sample size of the survey was important when determin-
ing prevalence of prehypertension. When the sample size was
less than 5 000 individuals, the pooled prevalence was observed
to be 36%. As the sample size increased, the prevalence rose
accordingly (39% for group of 5 000–10 000 individuals and
40% for group of
>
10 000). This positive correlation implies
an even higher prevalence of prehypertension among the world
population.
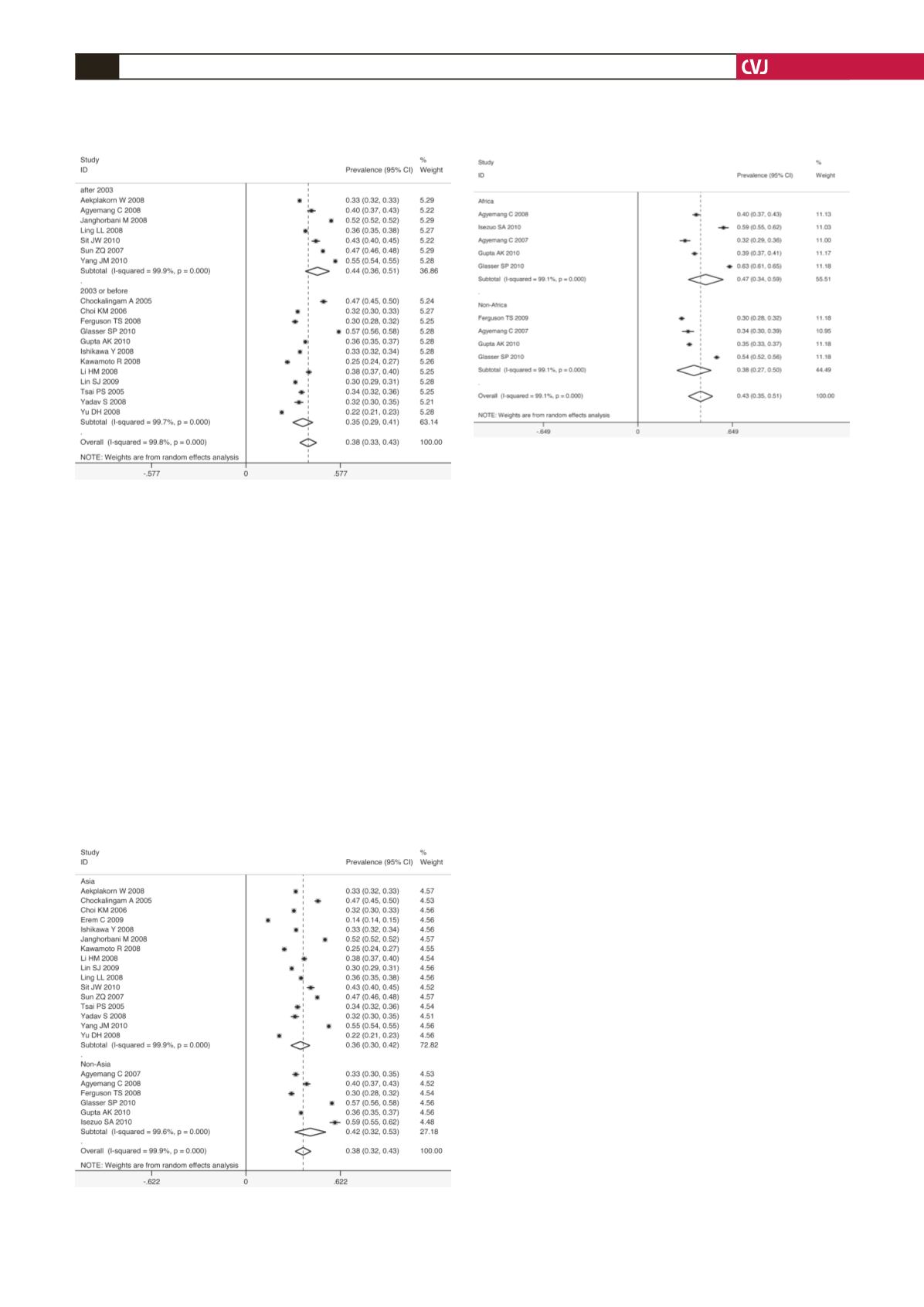
The year of inception of the survey was the only source of
heterogeneity we found in this pooled analysis. A sharp increase
in the prevalence of prehypertension was found after 2003 in the
subgroup analysis. Since the JNC7 introduced the term ‘prehy-
pertension’ in their 2003 report, this may have been one of the
factors increasing awareness of the risks related to prehyperten-
sion at the population level, particularly via the media and in
the public health community. In addition, changes in lifestyle in
recent years, which contribute to increased body mass, may also
result in the increased prevalence of prehypertension.
43-45
The reclassification of blood pressure levels in the new guide-
lines of the JNC7 in 2003 was prompted by several influential
epidemiological studies and clinical trials. It was necessary to
know the overall prevalence of prehypertension for the establish-
ment of the new guidelines and to indicate the importance of
prevention and treatment strategies among healthcare providers.
Morbidity and mortality as well as healthcare costs attributable
to prehypertension are substantial.
The rate of progression from prehypertension to clinical
hypertension, which depended on blood pressure level and age,
was 19% over four years.
46
Prehypertension was related to a
27% increase in all-cause mortality and a 66% increase in CVD
mortality.
47
In the NHANES-I cohort with a follow up of over 20
years, an estimated 3.4% of hospitalisations and 9.1% of deaths
could be attributed to prehypertension.
48
Unlike hypertensive patients, there is no evidence that
Fig. 10. Pooled prevalence grouped by African and non-
African population.
Fig. 8. Pooled prevalence grouped by inception year of
survey.
Fig. 9. Pooled prevalence grouped by Asian and non-
Asian population.