CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 7, August 2013
AFRICA
261
Myocardial protectionwas obtained by cold blood cardioplegic
solution. Patients were cooled to 32°C applying alpha-stat acid–
base management. Perfusion pressure was maintained in the
range of 40 to 70 mmHg.
Cardiac output (CO), cardiac index (CI), systemic vascular
resistance (SVR), pulmonary vascular resistance (PVR) and
mean pulmonary artery pressure (MPAP) were recorded for each
patient. Levosimendan (Simdax; Orion Corporation, Finland)
was administered to 10 patients following anaesthetic induction,
with a loading dose of 12
μ
g/kg administered in 10 minutes,
followed by a 24-hour infusion at a rate of 0.1
μ
l/kg/min (group
I). Ten patients to whom levosimendan was not administered
were regarded as the control group (group II).
Measurements were performed using a 7F Multiflex
thermodilution catheter (Abbot Laboratories, Hospital Products
Division, USA). Cold normal saline was administered through
the proximal end of the thermodilution catheter and sampling was
performed from the distal end of the catheter. Five measurements
were carried out for each parameter, minimum and maximum
values were excluded, and averages of the remaining values
were obtained. On the other hand, PVR and SVR values were
calculated and recorded by the computer system.
Following insertion of the thermodilution catheter after
general anaesthesia, initial values were recorded for all the
patients and these were regarded as baseline values (CO
1
, CI
1
,
SVR
1
, PVR
1
, and MPAP
1
). The rest of the measurements in the
levosimendan group were acquired following the administration
of the loading dose (CO
2
, CI
2
, SVR
2
, PVR
2
, MPAP
2
), at the
sixth hour of the levosimendan infusion (CO
3
, CI
3
, SVR
3
, PVR
3
,
MPAP
3
), at the 12th hour of levosimendan infusion (CO
4
, CI
4
,
SVR
4
, PVR
4
, MPAP
4
), and at 24th hour of the levosimendan
infusion (CO
5
, CI
5
, SVR
5
, PVR
5
, MPAP
5
). Measurements for the
control group were performed at equivalent periods.
Statistical analysis
Normally distributed continuous variables were expressed as
mean values
±
standard deviation (SD). Categorical variables
were expressed as numbers and percentages. Demographic
characteristics, peri-operative variables and calculated values
were compared using independent samples
t
-test for continuous
variables and the chi-square test or Fisher’s exact test for
categorical variables. Within-group differences were evaluated
with the paired-samples
t
-test. A
p
-value
<
0.05 was considered
statistically significant. All statistical analyses were performed
using the SPSS statistical software (SPSS for Windows 12.0,
Inc., Chicago, IL, USA).
Results
Demographic data of patients in the levosimendan and control
groups are shown in Table 1. There was no difference between
the two groups apart from body surface area values. In addition,
there was no difference between EuroSCORE values of groups
I and II (
p
=
0.418).
In group I, there were three patients with mitral regurgitation,
four with mitral stenosis and three with combined aortic stenosis
and mitral stenosis. On the other hand, in group II, there were six
patients with mitral stenosis, two with combined aortic stenosis
and mitral stenosis and two with prosthetic valve dysfunction.
Surgical procedures performed on both groups are summarised
in Table 2.
Duration of cross-clamp, CPB and surgery, dosage of inotropic
drugs, and the length of intensive care unit and hospital stay of
both groups are documented in Table 3. There was no significant
difference between cross-clamp, CPB and operation times. No
difference was detected for length of intensive care unit stay,
whereas it was found that the length of hospital stay for the study
group was significantly longer (group I: 7.8
±
2.4 days vs group
II: 5.8
±
1.5 days;
p
=
0.014). No marked adverse reaction to the
drug was observed in group I.
A statistically significant difference in favour of the
levosimendan group was recorded regarding the statistical values
of cardiac outputs and cardiac indexes between the two groups.
For baseline values, CO
1
values of group I were significantly
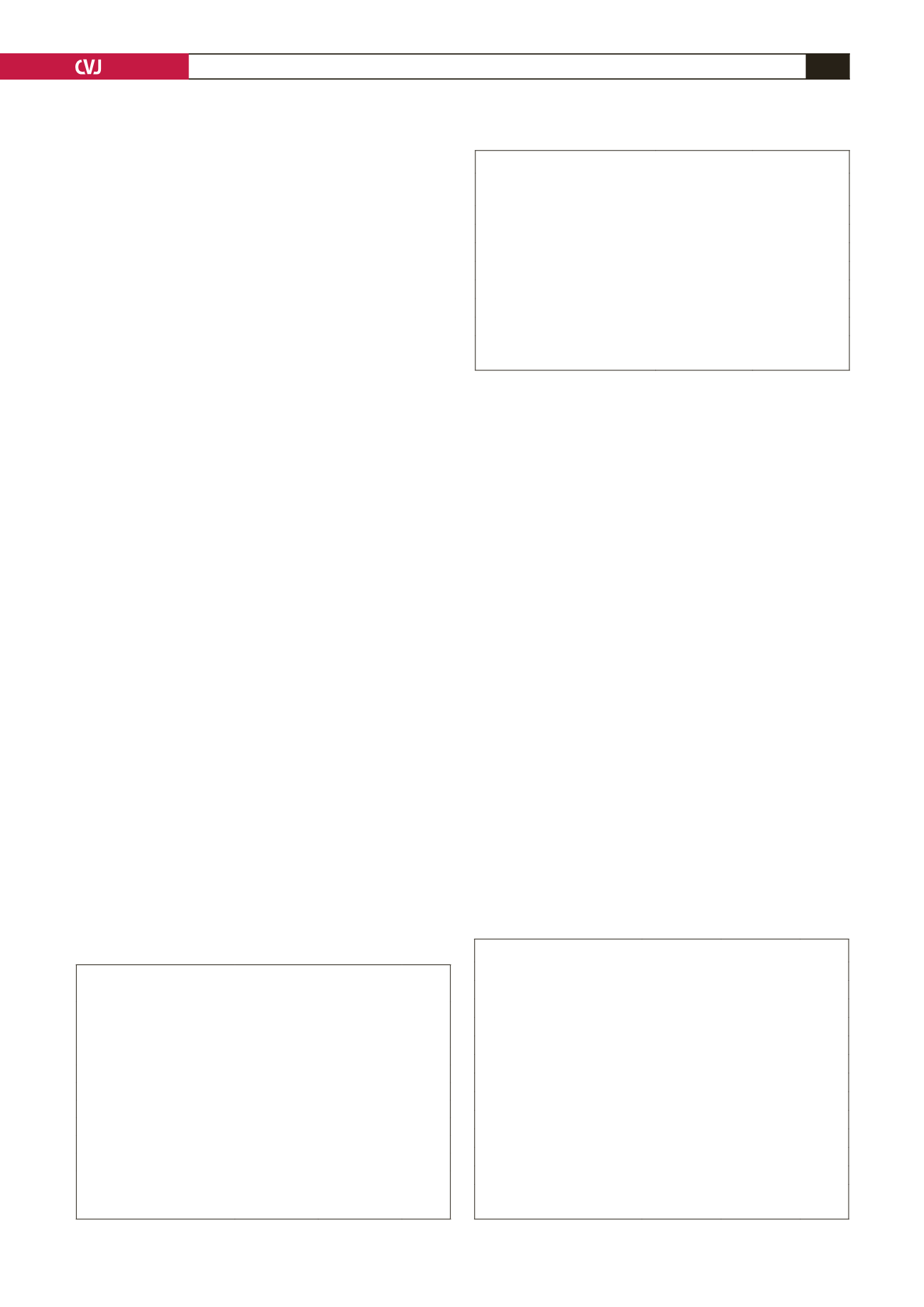
TABLE 1. COMPARISON OF DEMOGRAPHIC
DATA BETWEEN GROUPS
Characteristics
Group I
(levosimendan)
(
n
=
10)
Group II
(control)
(
n
=
10)
p
-value
Age (years)
49.6
±
10.7 45.7
±
7.9 0.125
Male/female
5/5
3/7
0.361
BSA (m
2
)
1.60
±
0.22 1.67
±
0.17 0.006
Functional capacity (NYHA)
3.2
±
0.6
3.4
±
0.5 1.000
Pre-operative EF (%)
46.8
±
10.9 49.0
±
12.0 0.182
COPD (+/–)
3/7
2/7
0.695
Pre-operative sPAP (mmHg)
71.2
±
23.6 72.8
±
15.8 0.151
BSA: body surface area, COPD: chronic obstructive pulmonary disease,
EF: ejection fraction, NYHA: NewYork Heart Association, sPAP: systolic
pulmonary arterial pressure.
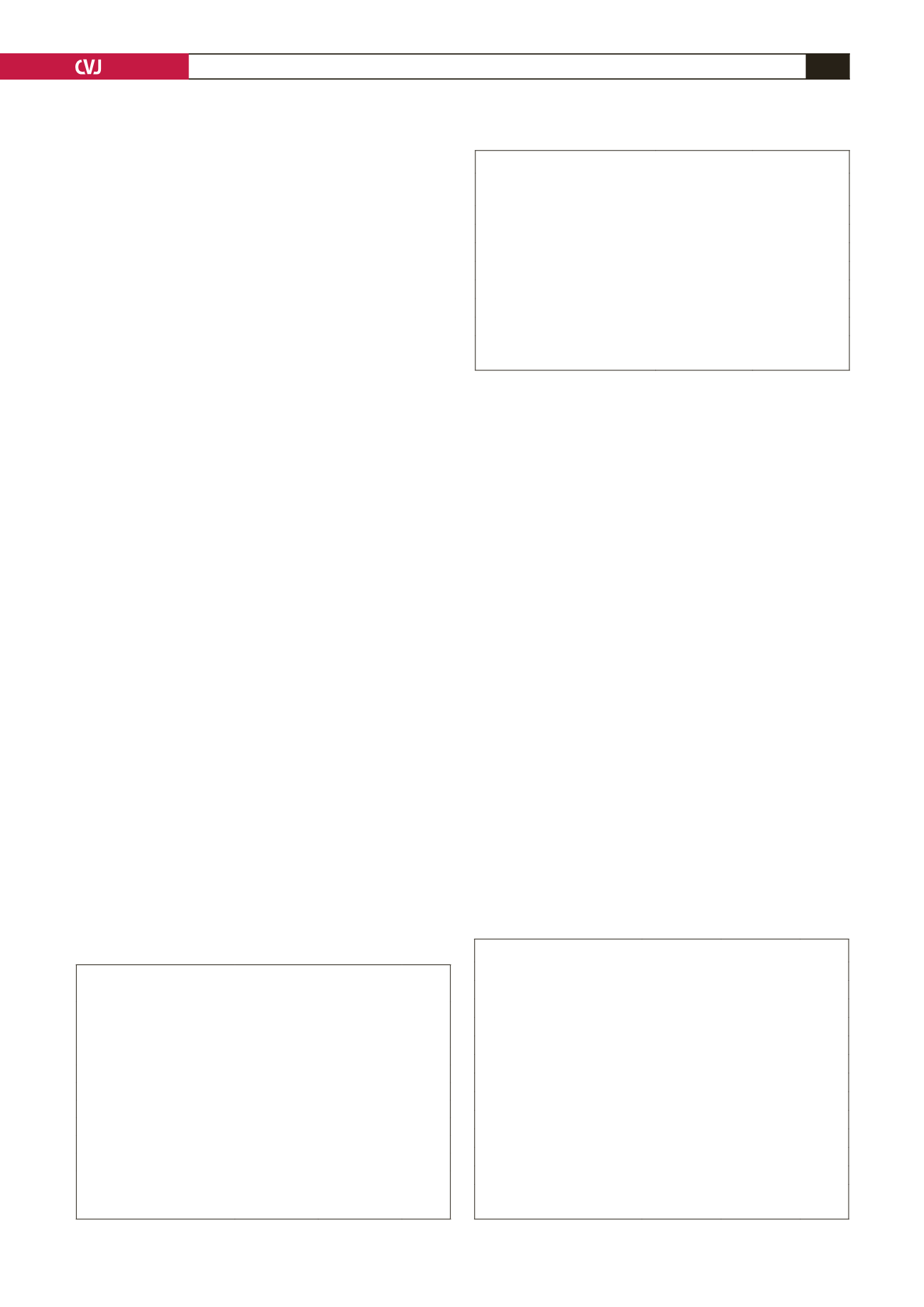
TABLE 2. SURGICAL PROCEDURES PERFORMED
Surgery type
Group I
(levosimendan)
Group II
(control)
MVR (redo)
2
2
MVR
2
4
AVR + MVR
3
2
Mitral repair
1
0
Mitral repair + CABG
2
0
AVR + MVR (redo AVR)
0
1
AVR + MVR (redo MVR)
0
1
MVR: mitral valve replacement, AVR: aortic valve replacement, CABG:
coronary artery bypass graft.
TABLE 3. INTRA- AND POSTOPERATIVE DATA
Features
Group I
Group II
p
-value
XCL period (min)
88.7
±
56.4 69.2
±
26.8 0.779
CPB period (min)
115.4
±
62.8 89.4
±
33.2 0.884
Operation time (min)
219.5
±
83.2 155.0
±
49.4 0.424
Need for inotropic drug
5
2
0.160
Need for IABP
0
0
–
Mortality
0
0
–
Postoperative exploration
0
0
–
Low cardiac output
0
0
–
Acute renal failure
0
0
–
Length of stay in ICU (days)
2.7
±
2.1
1.4
±
1.3 0.893
Length of stay at hospital (days)
7.8
±
2.4
5.8
±
1.5 0.012
XCL: cross-clamp, CPB: cardiopulmonary bypass; IABP: intra-aortic
balloon counterpulsation, ICU: intensive care unit.