
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 4, July/August 2015
178
AFRICA
A standardised, pre-tested questionnaire was used to collect
data on sociodemographic characteristics, medical history,
laboratory test parameters, electrocardiography (ECG) and
echocardiography variables, and physical signs, with an emphasis
on cardiovascular risk factors. Six traditional cardiovascular
risk factors, including male gender, older age, cigarette smoking,
obesity, diabetes mellitus, hypertension (defined according
to JNC 7),
9
and dyslipidaemia [elevated non-high-density
lipoprotein cholesterol > 130 mg/dl (3.37 mmol/l)], and two
non-traditional risk factors, anaemia and abnormal calcium/
phosphate metabolism were the focus of this study.
Laboratory tests focused on levels of creatinine, urea,
albumin, total cholesterol, triglycerides, high-density lipoprotein
(HDL) cholesterol, low-density lipoprotein (LDL) cholesterol,
phosphorus, calcium, haemoglobinandproteinuria.Haemoglobin
concentration was determined using Celltac E, an automated
CBC machine. Clinical chemistry tests were performed using
Cobas 6000, an automated analyser fromRoche pharmaceuticals.
Resting ECGs were carried out using the Schillar ECG
Recorder, (Basal, Switzerland). Echocardiograms were done
using the Vivid 7 Dimension, GE Medical Systems (Horten,
Norway) according to American Society of Echocardiography
guidelines. GFR was estimated for all study participants using
the Cockcroft–Gault equation. Non-HDL cholesterol and body
mass index were calculated using standard methods.
Statistical analyses
Data were double entered into epidata version 3.1 and exported
to STATA version 10 (after validation) for analysis. Results were
expressed as percentages and means with standard deviations,
and presented in tables and graphs. Chi-squared tests were used
to determine associations (declining renal function versus risk-
factor profiles). Results were statistically significant when the
p-
value was
<
0.05.
Results
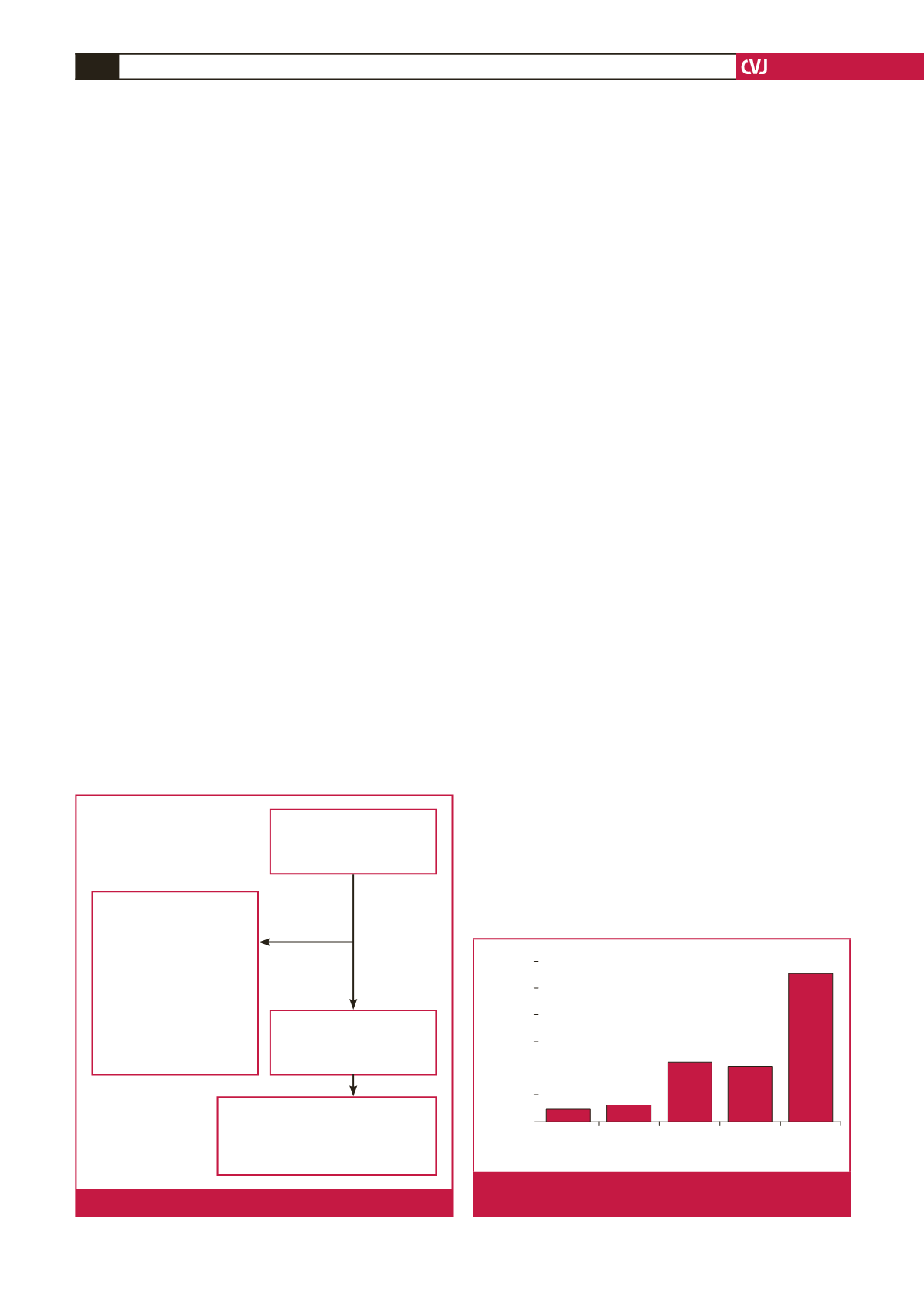
A total of 258 patients were screened over a period of nine
months. Forty-one were excluded from the study for various
reasons (Fig. 1). One hundred and eleven (51.2%) of the
participants were male. The mean age of study participants was
42.8 years (95% CI
=
40.6–44.9).
About half of the patients had ESRD (111, 51.2%) (Fig. 2). A
total of 184 patients (84.8%) had proteinuria. One hundred and
sixty-two subjects (74.65%) had had a non-reactive HIV antibody
test within the three months prior to recruitment, 32 patients
(14.75%) were HIV positive, and the remaining 23 (10.60%) had
had no evidence for taking the HIV test in the previous three
months. The patient characteristics are summarised in Table 1.
Twenty-five patients (11.5%) were either current smokers
or had a history of tobacco smoking. There was a higher
prevalence of cigarette smoking among males (18.9 vs 3.8) and
this was statistically significant (
p
<
0.001). The prevalence of
hypertension was 90%, with 88% of patients on treatment but
only 24% had their blood pressure under control (Table 2).
Diabetes prevalence was 16.1% and 22 patients (10.1%) were
obese (BMI ≥ 30 kg/m²). Despite the fact that 89 patients (41%)
had elevated non-HDL cholesterol of ≥ 130 mg/dl (3.37 mmol/l),
only nine patients (4.2%) were on statin lipid-lowering therapy.
One hundred and fifty-six patients (71.9%) had haemoglobin
concentrations
<
11 g/dl. Only three patients (1.4%) were on
weekly anaemia treatment with erythropoietin and iron sucrose,
as recommended by the United States NKF-KDOQI. A large
proportion, 156 patients (71.9%) were on oral iron and folate
therapy.
Ninety-seven patients (44.70%) were found to have
hypocalcaemia (calcium
<
2.2 mmol/l) and 85 (39.17%) had
serum phosphate concentrations above the reference range (0.9–
1.5 mmol/l). The cardiovascular risk factors are summarised in
Table 2.
All study participants underwent resting ECG and
two-dimensional echocardiography. Echocardiographically
determined left ventricular hypertrophy (interventricular septum
and/or left ventricular posterior wall thickness > 11 mm in
diameter) was present in 54% of the participants, followed by
left ventricular systolic failure (ejection fraction
<
45%) in 19.4%.
Ischaemic heart disease and malignant cardiac arrhythmias were
less common (Fig. 3).
41 were excluded:
8 did not meet inclusion
criteria
• 3 declined to consent
• 2 had deranged renal
function for less than 3
months.
• 2 were less than 18
years of age
• 1 was a dialysis patient
33 did not return for
further tests.
Participants were evaluated
for cardiovascular risk factors
through medical history/physical
examination and laboratory tests
217 patients were
eligible and included
in the final analysis
258 patients screened in
the renal clinic
(June 2012 – Feb 2013)
Fig. 1.
Patient flow chart.
120
100
80
60
40
20
0
1
2
3
4
5
Stage of CKD
No of cases
Fig. 2.
Graph showing distribution of patients by stage of
chronic kidney disease (CKD).

















