
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
92
AFRICA
mechanism of pregnancy, aiming at preventing pregnant women
from consuming potentially teratogenic substances such as
strong-tasting fruits and vegetables. The exact underlying
mechanism is not clear but pregnancy-associated hormones
such as human chorionic gonadotropin (hCG), oestrogen and
progesterone could to be involved in the aetiology. The levels of
hCG peak at the end of the first trimester when the trophoblast
is most actively producing hCG, correlating with the nausea
symptoms. Nausea is also more frequent in pregnancies with
high levels of hCG, such as in twin pregnancies.
Thyroid hormones may also be involved in the development
of nausea symptoms, as a strong association with nausea and
abnormal thyroid function tests has been found. Thyroid-
stimulating hormone (TSH) and hCG have similar biomolecular
structures and therefore hCG cross-reacts with TSH, stimulating
the thyroid gland.
18
Psychological causes, genetic incompatibility,
immunological factors, nutritional deficiencies as well as
Helicobacter pylori
infection have been proposed as aetiological
factors of nausea and vomiting during pregnancy.
20
The nausea symptoms usually resolve by week 20 but
about 10–20% of the patients experience symptoms beyond
week 20 and some until the end of the pregnancy.
21
In most
cases minor dietary modification and observation of electrolyte
balance is sufficient. About 0.5–3% of pregnant women develop
hyperemesis gravidum, a severe form of nausea and excessive
vomiting, often resulting in dehydration, electrolyte imbalance,
ketonuria, weight loss and vitamin or mineral deficiencies.
19,21
In these cases intravenous fluid and vitamin substitution is
commonly required. Thiamine supplementation is important in
order to avoid the development of Wernicke’s encephalopathy.
22
As pregnancy progresses, mechanical changes in the
alimentary tract also occur, caused by the growing uterus. The
stomach is increasingly displaced upwards, leading to an altered
axis and increased intra-gastric pressure. The oesophageal
sphincter tone is also decreased and these factors may predispose
to symptoms of reflux, as well as nausea and vomiting.
23
Changes in oestrogen and progesterone levels also influence
the structural alterations in the gastrointestinal tract. These
include abnormalities in gastric neural activity and smooth
muscle function, leading to gastic dysrhythmia or gastroparesis.
The alterations are pronounced in women with pre-existing
gastrointestinal diseases such as gastroesophageal reflux disease,
diabetic gastroparesis, gastric bypass surgery or inflammatory
bowel disease.
21,23
Endocrine changes
Thyroid
There is an increase in the production of thyroxine-binding globulin
(TBG) by the liver, resulting in increased levels of thyroxine (T
4
)
and tri-iodothyronine (T
3
). Serum free T
4
(fT
4
) and T
3
(fT
3
) levels
are slightly altered but are usually of no clinical significance. Levels
of free T
3
and T
4
do however decrease slightly in the second and
third trimesters of pregnancy and the normal ranges are reduced.
24
Free T
3
and T
4
are the physiologically important hormones and are
the main determinants of whether a patient is euthyroid.
Serum concentrations of TSH are decreased slightly in the
first trimester in response to the thyrotropic effects of increased
levels of human chorionic gonadotropin. Levels of TSH increase
again at the end of the first trimester, and the upper limit in
pregnancy is raised to 5.5 μmol/l compared with the level of 4.0
μmol/l in the non-pregnant state (Table 2).
Pregnancy is associated with a relative iodine deficiency. The
causes for this are active transport of iodine from the mother
to the foeto-placental unit and increased iodine excretion in the
urine. The World Health Organisation recommends an increase
in iodine intake in pregnancy from 100 to 150–200 mg/day.
24
If
iodine intake is maintained in pregnancy, the size of the thyroid
gland remains unchanged and therefore the presence of goiter
should always be investigated. The thyroid gland is 25% larger in
patients who are iodine deficient.
Adrenal gland
Three types of steroids are produced by the adrenal glands:
mineralocorticoids, glucocorticoids and sex steroids. The RAA
system is stimulated due to reductions in vascular resistance and
blood pressure, causing a three-fold increase in aldosterone levels
in the first trimester and a 10-fold increase in the third trimester.
25,26
Levels of angiotensin II are increased two- to four-fold and renin
activity is increased three to four times that of non-pregnant values.
During pregnancy there is also an increase in serum levels
of deoxycorticosterone, corticosteroid-binding globulin (CBG),
adrenocorticotropic hormone (ACTH), cortisol and free cortisol.
These changes cause a state of physiological hypercortisolism and
may be clinically manifested by the striae, facial plethora, rising
blood pressure or impaired glucose tolerance.
27
Total cortisol levels
increase at the end of the first trimester and are three times higher
than non-pregnant values at the end of pregnancy. Hypercortisolism
in late pregnancy is also the result of the production of corticotropin-
releasing hormone by the placenta – one of the triggers for the onset
of labour. Diurnal variations in ACTH and cortisol levels are
maintained. The hypothalamic–pituitary axis response to exogenous
glucocorticoids is blunted during pregnancy.
Table 2. Reference ranges for thyroid function in pregnancy
37
Thyroid function
Non-
pregnant
1st
trimester
2nd
trimester
3rd
trimester
fT
4
(pmol/l)
9–26
10–16
9–15.5
8–14.5
fT
3
(pmol/l)
2.6–5.7
3–7
3–5.5
2.5–5.5
TSH (mU/l)
0.3–4.2
0–5.5
0.5–3.5
0.5–4
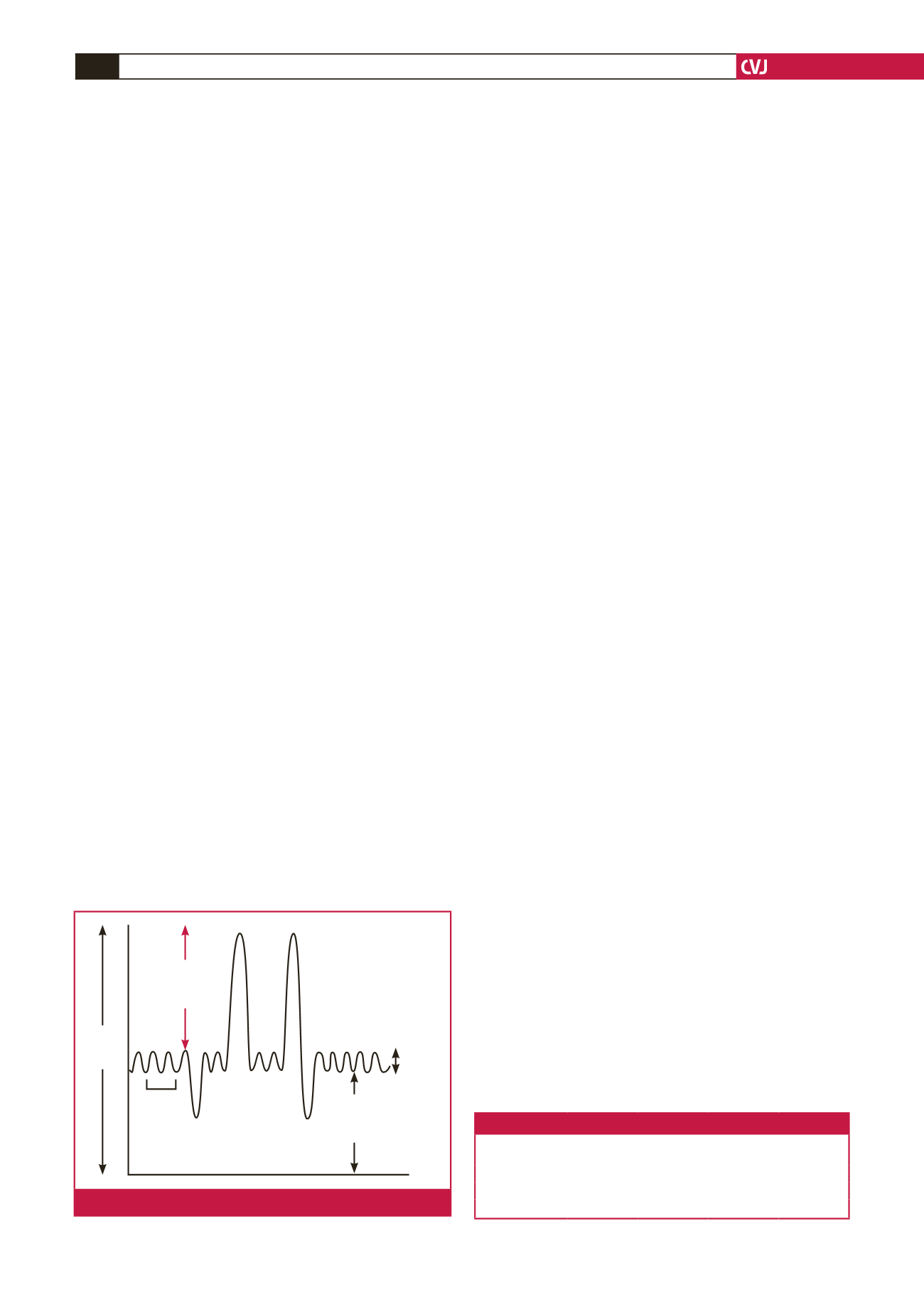
Lung
volume
(ml)
Inspiratory
reserve
volume
Functional
residual
capacity
Tidal
volume
Respiratory
rate
Fig. 1.
Physiological changes in respiratory function in pregnancy.

















