
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 4, July/August 2016
244
AFRICA
Statistical analysis
The Statistical Package for Social Sciences program version 16.0
(SPSS Inc, Chicago, IL, USA) was used. Descriptive data were
expressed as mean, standard deviation and range (minimum
to maximum values). Numbers and percentiles were used for
expression of categorical variables. Parametric tests were used
for data with a normal distribution, and non-parametric tests
were applied to data without a normal distribution.
Distribution of normality was tested with the Kolmogorov–
Smirnov test. The Mann–Whitney
U
- and Wilcoxon tests were
used for comparing variables between groups. Chi-squared,
Fisher’s and Mantel Haenszel tests were performed for
comparison of categorical variables. Level of significance was
set at
p
<
0.05.
Results
The study group consisted of a total of 20 patients (3 females, 17
males) with average ages of 61.7
±
13.2 years (range, 44–78) and
63.1
±
9.6 years (range, 51–78), for groups 1 and 2, respectively.
The descriptive data and peri-operative characteristics are shown
in Table 1.
The average values for serum albumin, total protein, C3c and
C4 levels were higher in group 1 at the start of the pump (Table
2). No difference was observed between the groups in terms of
these variables at the end of CPB (Table 2). In group 1, total
protein levels were significantly higher at the start of the pump
compared to at the end of CPB (
p
=
0.01). A significantly lower
IgG level was noted at the end of CPB compared to at the start
in group 1 (
p
=
0.012) (Table 2).
IgM levels at the end of CPB were higher than IgM levels at
the start in group 1 (
p
=
0.012). In group 1, mean levels of C3c
were lower at the end of CPB compared to those at the start (
p
=
0.005) (Table 2).
Discussion
In this study, we attempted to demonstrate whether there was
a difference between the cellular immune responses of patients
who underwent CPB using uncoated or phosphorylcholine-
coated oxygenators. Our study indicated that a more prominent
cellular immune response was observed in patients operated on
using phosphorylcholine-coated oxygenators.
In spite of the advantages it offers during cardiac surgery,
CPB has the potential to cause a complex inflammatory response,
initiated by the contact of heparinised bloodwith non-endothelial
surfaces.
6
Other factors, such as bleeding, ischaemia–reperfusion
injury and rejection reactions further contribute to augmentation
of the immune response via secretion of vasoactive and cytotoxic
cytokines, resulting in alleviation of this inflammatory cascade.
2-5
Recently, modification of the surfaces that come into contact
with extracorporeal circulating blood has become popular and
phosphorylcholine is one of the materials used for this purpose.
7
In the literature, there are several reports on the impact of
coated oxygenators on the immune response. It was suggested
that leukocyte levels increased and platelet levels decreased in
both phosphorylcholine-coated and uncoated oxygenators with
regard to baseline values during induction of anaesthesia.
8,9
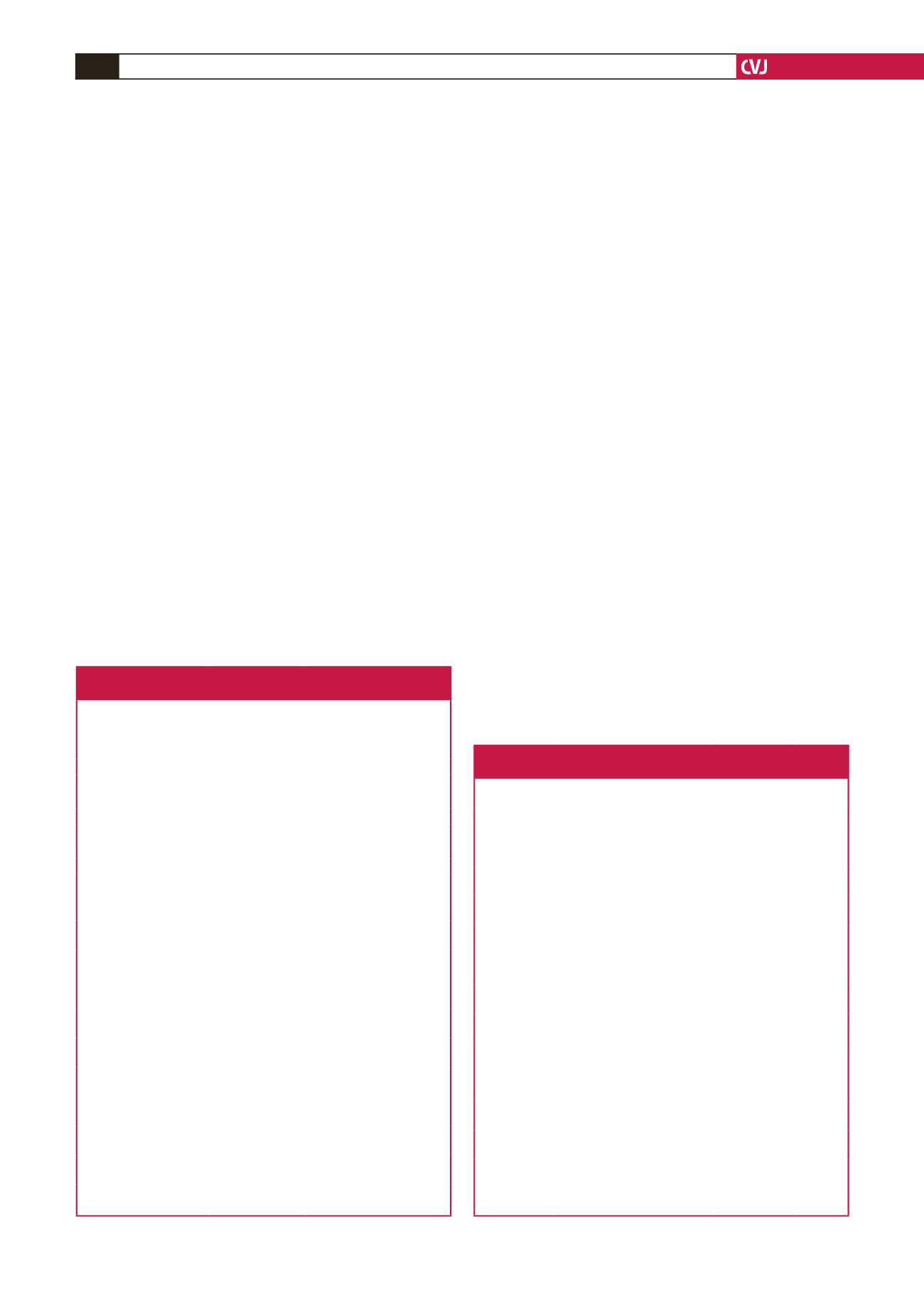
Table 1. Descriptive and peri-operative parameters
of the patients in groups 1 and 2
Parameters
Group 1
(
n
=
10)
Group 2
(
n
=
10)
p-
value
Age (years), median
(range)
61.7
±
13.25
(44–78)
63.1
±
9.64
(51–78)
0.677
Gender (M/F),
n
(%)
8/2 (80/20)
9/1 (90/10)
0.531
Risk factors
Diabetes mellitus,
n
(%)
2/8 (20/80)
3/7 (30/70)
1.000
Hypertension,
n
(%)
6/4 (60/40)
6/4 (60/40)
1.000
COPD,
n
(%)
1/9 (10/90)
2/8 (20/80)
1.000
CRF,
n
(%)
1/9 (10/90)
2/8 (20/80)
1.000
Smoking habit,
n
(%)
5/5 (50/50)
7/3 (70/30)
0.361
Ejection fraction (%),
median (range)
53.00
±
3.58
(30–65)
47.08
±
10.30
(30–65)
0.193
Postoperative features
Duration of cross clamp
(min), median (range)
49.60
±
13.67
(30–77)
58.70
±
23.55
(40–113)
0.405
Duration of CPB (min),
median (range)
88.40
±
26.28
(58–134)
102.1
±
25.58
(75–146)
0.162
Heparin (units/ml),
median (range)
4.20
±
0.42
(4–5)
5.50
±
0.84
(4–7)
0.001
Protamine (mg), median
(range)
4.60
±
0.51
(4–5)
5.70
±
1.05
(4–8)
0.008
Duration of intubation
(h), median (range)
8.00
±
2.90
(4–12)
9.4
±
3.74
(4–18)
0.488
ICU stay, (h), median
(range)
34.00
±
11.50
(20–48)
38.00
±
11.19
(24–48)
0.384
Hospitalisation (days),
median (range)
6.60
±
0.96
(6–9)
8.00
±
1.88
(6–12)
0.039
Drainage (ml), median
(range)
645.00
±
319.24
(200–1300)
530.00
±
182.87
(250–900)
0.447
Transfusion (units),
median (range)
920.00
±
454.11
(600–1800)
900.00
±
391.57
(600–1800)
0.934
M: male; F: female; CRF: chronic renal failure; COPD: chronic obstructive
pulmonary disease; CPB: cardiopulmonary bypass; ICU: intensive care unit.
Table 2. Levels of total protein, serum albumin, IgG, IgM, and
complements C3c and C4.
Variable
Time of
measurement
Group 1
median (range)
Group 2
median (range)
p-
value
Total protein
(mg/dl)
Start of pump 3.36
±
0.31
(2.9–3.8)
4.08
±
0.57
(3.1–4.7)
0.009
§
End of pump 3.82
±
0.61
(3.1–4.8)*
4.16
±
0.37
(3.7–4.6)
0.223
Albumin (g/dl) Start of pump 1.96
±
0.08
(1.9–2.1)
2.14
±
0.31
(1.6–2.4)
0.030
§
End of pump 2.24
±
0.28
(1.9–2.7)*
2.24
±
0.23
(1.9–2.5)
0.758
IgG (g/l)
Start of pump 6.06
±
1.71
(3.5–7.8)
7.94
±
3.55
(3.6–12.4)
0.172
End of pump 7.48
±
1.96
(4.9–10.3)*
6.72
±
2.94
(3.2–9.9)
0.448
IgM (mg/l)
Start of pump 0.48
±
0.13
(0.43–0.72)
0.64
±
0.27
(0.21–0.98)
0.095
End of pump 0.54
±
0.14
(0.39–0.73)*
0.55
±
0.17
(0.23–0.68)
0.798
C3c (mg/dl)
Start of pump 0.58
±
0.11
(0.4–0.7)
0.81
±
0.19
(0.59–1.12)
0.010
§
End of pump 0.69
±
0.10
(0.54–0.82)*
0.73
±
0.07
(0.61–0.79)
0.601
C4 (mg/dl)
Start of pump 0.13
±
0.06
(0.08–0.23)
0.16
±
0.02
(0.13–0.19)
0.022
§
End of pump 0.29
±
0.31
(0.09–0.87)
0.18
±
0.04
(0.12–0.24)
0.315
IgG: immunoglobulin G; IgM: immunoglobulin M; C3c: complement factor
C3c; C4: complement c4.
*Statistically significant difference within the same group;
§
statistically signifi-
cant difference between the two groups.

















