
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 6, November/December 2016
AFRICA
379
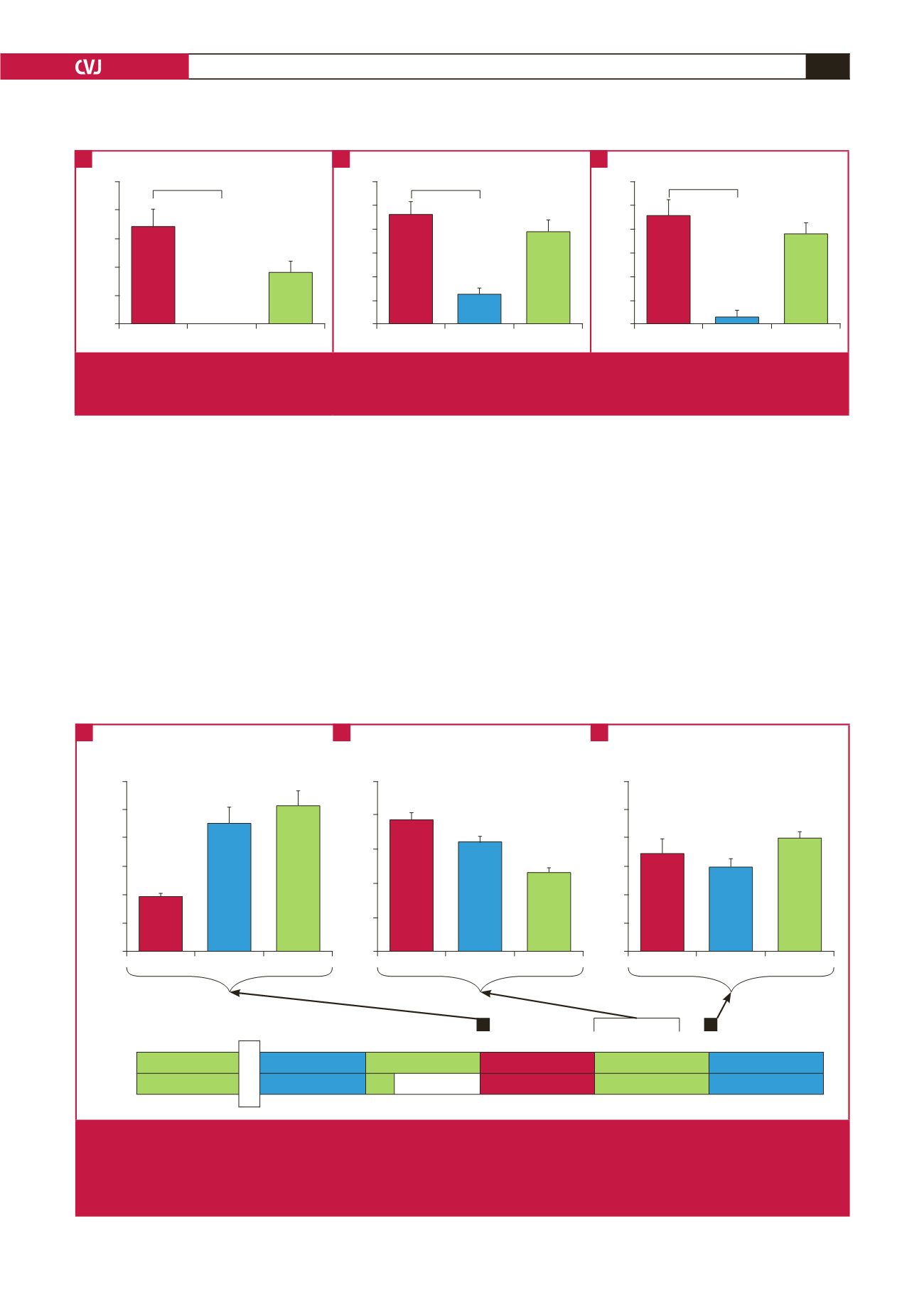
Surprisingly, at a dose of 2.5
µ
M, FTY720 administered as a
pre-treatment potently suppressed all functional recovery (Fig.
4), as evident by the fact that of the six hearts pre-treated with
FTY720, only one recovered sufficiently to generate recordable
total work data (aortic output: control: 33.88
±
6.12% vs PreFTY:
0%,
n
=
6–10;
p
<
0.001; cardiac output: control: 45.94
±
5.57%
vs PreFTY: 12.20
±
2.68%,
n
=
6–10;
p
<
0.001; and total work:
control: 45.67
±
8.98% vs PreFTY: 2.79%,
n
=
4–5;
p
<
0.01).
In view of this severe suppression of post-ischaemic function,
we also analysed heart rate (percentage recovery: control: 85.00
±
6.11% vs PreFTY: 10.53%,
n
=
6–8;
p
<
0.001) as well as systolic
pressure (percentage recovery: control: 88.13
±
4.45% vs PreFTY:
15.10%,
n
=
6–8;
p
<
0.001). We found both to be significantly
reduced in the FTY720 pre-treatment group.
During the perfusion experiments we noticed that FTY720
elicited a profound increase in coronary flow (CF) (Figs 5, 6).
Expression of CF at the end of pre-ischaemic drug administration
relative to retrograde perfusion stabilisation values (Fig. 5)
shows that both doses increased CF when administered prior to
ischaemia [control: 0.95
±
0.05 arbitrary units (AU) vs PreFTY
(1
µ
M): 2.25
±
0.27 AU and PreFTY (2.5
µ
M): 2.56
±
0.27
AU,
n
=
5–8;
p
<
0.01]. Expression of reperfusion CF relative
to pre-ischaemic stabilisation CF reveals a similar trend when
FTY720 was administered at the onset of reperfusion [Fig. 6;
control: 1.21
±
0.11 AU vs PostFTY (1
µ
M): 2.59
±
0.18 AU and
PostFTY (2.5
µ
M): 2.19
±
0.15 AU,
n
=
4–9;
p
<
0.01].
Surprisingly, the vasodilatory effect of FTY720 pre-treatment
(Fig. 5) was replaced by a reduction in CF during the first 15
minutes of reperfusion relative to the control [CF expressed
relative to retrograde stabilisation: control: 1.94
±
0.17 AU vs
Control
PreFTY PostFTY
Functional recovery
50
40
30
20
10
0
p
<
0.001
Control
PreFTY PostFTY
Functional recovery
60
50
40
30
20
10
0
p
<
0.001
Control
PreFTY PostFTY
Functional recovery
60
50
40
30
20
10
0
p
<
0.001
Fig. 4
The effect of FTY720 (2.5
μ
M) administered as either pre-treatment (PreFTY) or immediately following ischaemia (PostFTY)
on functional recovery. Pre-ischaemic administration of FTY720 was associated with a profound suppression of functional
recovery in terms of (A) aortic output, (B) cardiac output, and (C) total work,
n
=
4–10.
A
B
C
Control
1
μ
M FTY 2.5
μ
M FTY
Coronary flow ratio
1.50
1.25
1.00
0.75
0.50
0.25
0.00
Control
1
μ
M FTY 2.5
μ
M FTY
Coronary flow ratio
3.0
2.5
2.0
1.5
1.0
0.5
0.0
@
@
Coronary flow at the end of 15-minute drug
administration relative to stabilisation
Average coronary flow over the first 15 minutes
of reperfusion relative to stabilisation
Coronary perfusion at the end of retrograde
reperfusion relative to stabilisation
Control
1
μ
M FTY 2.5
μ
M FTY
Coronary flow ratio
2.5
2.0
1.5
1.0
0.5
0.0
@
@
Retrograde
Work
Retrograde
Ischaemia
Retrograde
Work
Control
15
15
20
20 GI
20
15
PreFTY
15
15
15 FTY
20 GI
20
15
stabilisation
Fig. 5
The effect of pre-treatment with FTY720 on coronary flow (CF) in a model of global ischaemia. Coronary flow was collected
during retrograde perfusion at the end of stabilisation, the end of drug administration and every two minutes for the first 15
minutes of reperfusion, as well as at the end of retrograde reperfusion. For comparison purposes, the CF of each time point
was expressed relative to the stabilisation values of that group. FTY720 increased CF during administration of the drug, but
reduced CF during initial reperfusion.
@
p
<
0.05 vs control,
n
=
3–11.
A
B
C

















