
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 3, May/June 2017
e6
AFRICA
<
0.01, 0.13,
<
0.01 ng/ml, respectively). Echocardiographic
examination revealed no obvious heart disease, wall motion
abnormalities or pericardial effusion.
As the patient’s chest pain was exertional, persistent and
angina-like, in conjunction with the ECG findings and troponin
levels, coronary artery imaging with multi-detector computed
tomography (MDCT) was performed. Coronary myocardial
bridging with a length of 12 mm was found in the middle tract
of the left anterior descending artery (LAD) (Figs 2, 3). For
the assessment of myocardial perfusion, magnetic resonance
imaging (MRI) was performed. Reduced perfusion of segments
seven and 12, consonant with ischaemia, and weak contrast
uptake, consonant with sub-endocardial infarct, were detected.
These lesions matched the areas supplied by the bridged segment
of the LAD that was defined by MDCT.
The chest pain was relieved with aspirin and beta-blocker
(metoprolol) therapy after the second day of admission. In
the following days, the patient was asymptomatic, the cardiac
enzymes were all within the normal range, and the initial ECG
changes were attenuated (Fig. 4). A 24-hour Holter monitor
demonstrated neither ectopic beats nor tachyarrhythmias. An
exercise stress test, based on the Bruce protocol, revealed no
ischaemic changes or arrhythmias.
The patient was restricted from strenuous exertion.
Metoprolol was prescribed and the patient was discharged
without any problems. We decided to remove the bridge surgically
if he becomes symptomatic despite physical restriction and drug
therapy. After the six-month follow up, the patient had no
cardiac symptoms and his ECG remained normal.
Discussion
Early repolarisation is defined as either a sharp, well-defined
positive deflection or notch immediately following a positive
QRS complex at the onset of the ST segment, or the presence
of slurring at the terminal part of the QRS complex. Several
population studies have estimated that the prevalence of early
repolarisation ranges from five to 13% of persons.
5,6
‘Early repolarisation pattern’ describes the patient with
appropriate ECG findings in the absence of symptomatic
arrhythmias. On the other hand, ‘early repolarisation syndrome’
applies to the patient with both appropriate ECG findings and
symptomatic arrhythmias. Large population studies have shown
that the presence of early repolarisation in the inferior leads
on surface ECG is associated with an increased risk of death
from cardiac causes as well as all-cause mortality.
2,3
Our patient
had early repolarisation pattern in the inferior leads with no
documented arrhythmia.
Early repolarisation pattern may be seen in secondary
conditions such as hypothermia, autonomic nervous system
disturbances, cocaine abuse, antidepressant use, hypercalcaemia,
neuropsychiatric disturbances, subarachnoid haemorrhage,
metabolic diseases and cardiac diseases (acute coronary
syndrome, myocardial ischaemia, hyper-vagotony, hypertrophic
cardiomyopathy and pericarditis–myocarditis). Numerous benign
and less life-threatening diseases such as early repolarisation,
acute pericarditis and vasospastic angina can present with chest
pain. ST-segment elevation on an electrocardiogram may occur
in all these situations and many others, creating a diagnostic
dilemma.
Originally considered to be a benign entity, recent reports
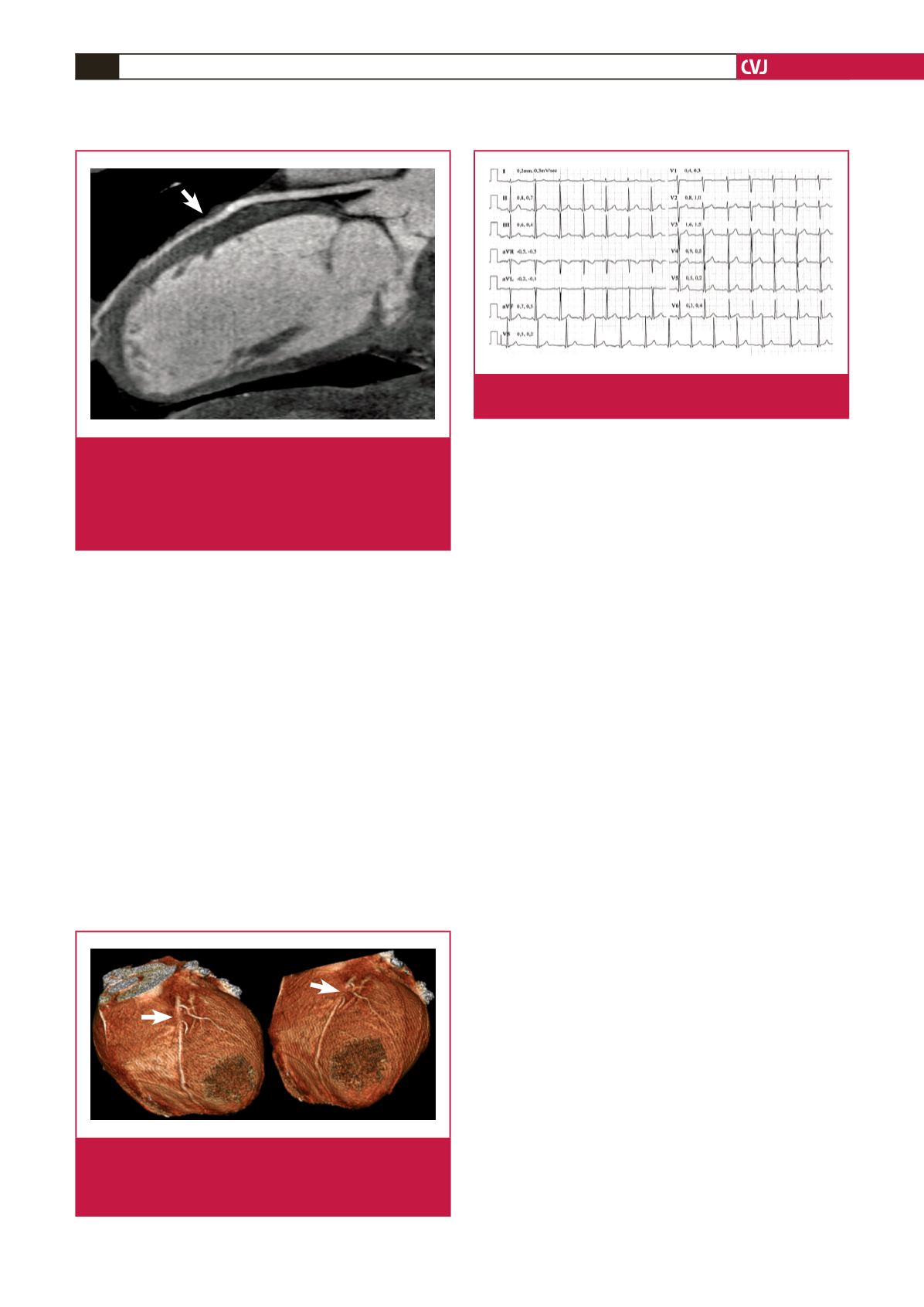
Fig. 3.
Three-dimensional volume-rendered image in which
the myocardial bridging covers the upper middle
segment of the LAD coronary artery. The arrow indi-
cates the location of myocardial bridging.
Fig. 2.
ECG-gated coronary CT angiography of the patient
performed with 64-MDCT. A curved multi-planar refor-
mat image shows a 12-mm bridging of the mid-
segment of the LAD. The arrow indicates the location
of myocardial bridging. MDCT, multi-detector comput-
ed tomography; LAD, left anterior descending artery.
Fig. 4.
ECG at a baseline exercise-stress test on the seventh
day of admission shows no abnormality
.

















