
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 5, September/October 2017
AFRICA
311
coronary artery disease and atrial fibrillation) (Table 1), and
laboratory results, including cardiac enzymes, except for D-dimer
values. In addition, echocardiographic characteristics were not
significantly different between the two groups.
Similarly, RV FAC, RVs
′
and TAPSE values, known as
measures of RV function, did not differ significantly between
the two groups. Table 3 compares the RV strain values of the
two groups. RV GLS values of all patients were lower than
the normal range (approximately –28.0%.)
14,15
RV GLS values
of patients in the group with pulmonary complications were
significantly lower than those of patients in the group with no
complications (–12.40
±
6.41 vs –17.14
±
5.72 %,
p
=
0.036). With
regard to segmental RV strain values, the apico-septal RV strain
of patients in the group with pulmonary complications was
noticeably worse than that in the group with no complications
(–3.38
±
12.98 vs –16.61
±
11.04%,
p
=
0.010).
In univariate analyses (Table 4), worse RV GLS values were
associated with pulmonary complications in patients [odds ratio
(OR) 1.17, 95% confidence interval (CI) 1.007–1.369,
p
=
0.040].
Duration of hospital stay was also associated with pulmonary
complications [OR 1.17, 95% CI: 1.041–1.307,
p
=
0.008].
Furthermore, in multivariate regression analyses, worse RV GLS
values were independent predictors of pulmonary complications
after adjustment for other relevant variables in patients [OR 2.09,
95% CI: 1.047–4.151,
p
=
0.037]. In addition, longer hospital stay
was an independent predictor of pulmonary complications [OR
1.64, 95% CI: 1.053–2.560,
p
=
0.029].
ROC curve analysis identified RV GLS of –14.85% as the best
cut-off value for predicting pulmonary complications; this value
had a sensitivity of 75.0% and a specificity of 62.9% (Fig 1). Fig.
2 shows the cumulative clinical event-free survival rates of the
two groups during the one-month postoperative period. The two
groups were stratified by a RV GLS value of –14.85%. Patients
with RV GLS values
>
–14.85% had a significantly higher rate of
pulmonary complications during the first postoperative month
than did patients whose RV GLS was ≤ –14.85% (log-rank test:
p
=
0.027). Based on univariate cox regression analysis, RV GLS
values
>
–14.85% had borderline significance for the prediction
of pulmonary complications [hazard ratio (HR) 7.60, 95% CI:
0.912–63.459,
p
=
0.061] during the one-month postoperative
period (data are not shown).
The inter-observer agreement of RV GLS was excellent
(ICC 0.987, 95% CI: 0.966–0.995, respectively). The degree of
intra-observer agreement (ICC 0.989, 95% CI: 0.973–0.996) was
similar to that of the inter-observer agreement.
Discussion
Pneumonia and pulmonary embolism are important
complications in older patients with femur fracture. Our findings
indicate that pulmonary complications develop often, at a rate
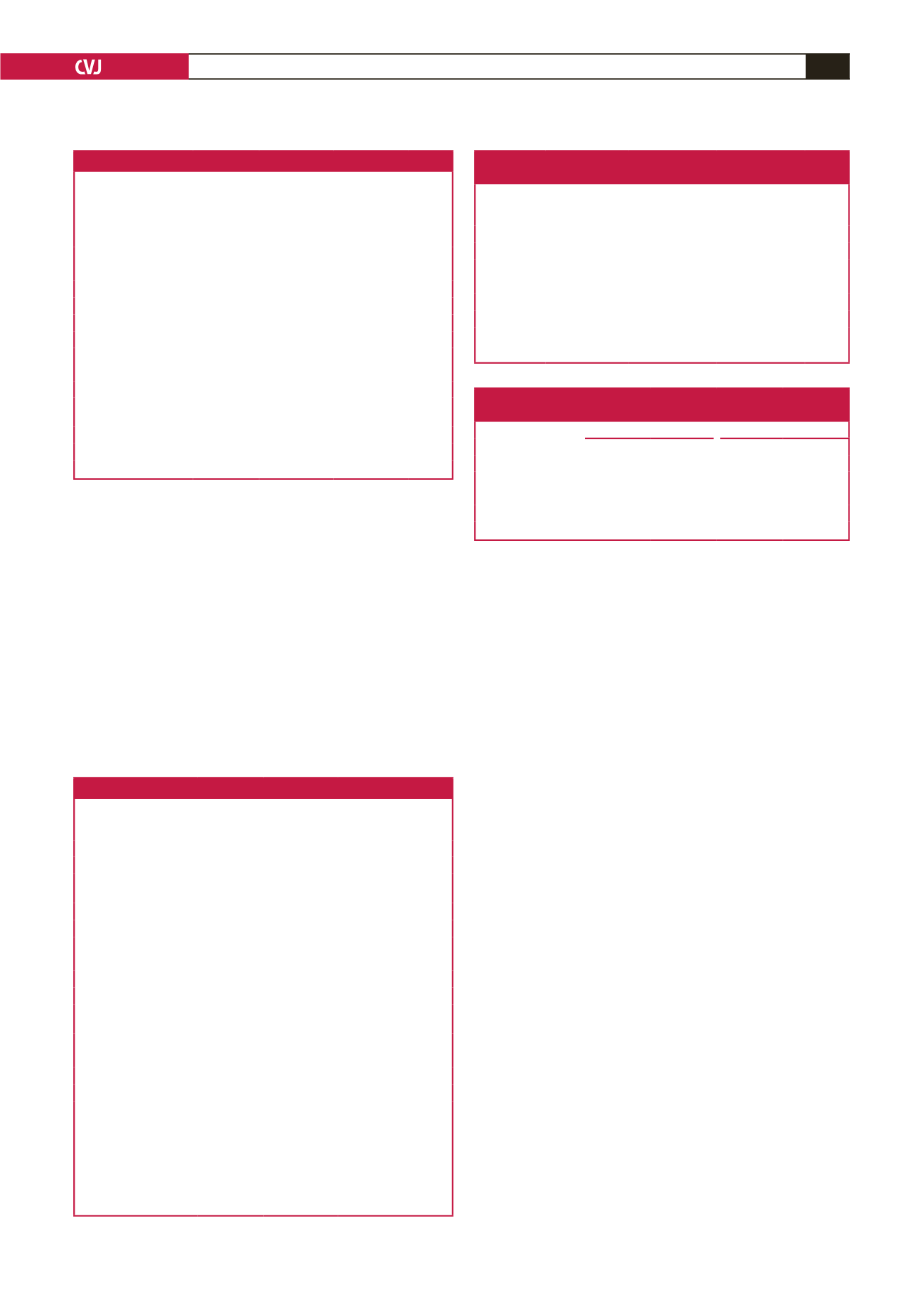
Table 1. Baseline characteristics
Clinical variables
All (
n
=
78)
Pulmonary
complications
(
n
=
8)
No
complications
(
n
=
70)
p
-value
Age, years
80.1
±
9.1 83.4
±
3.2
79.7
±
9.5 0.310
Females,
n
(%)
59 (75.6)
5 (62.5)
54 (77.1)
0.395
SBP, mmHg
128.5
±
20.6 126.5
±
23.3 128.8
±
20.5 0.728
DBP, mmHg
74.7
±
11.9 71.9
±
8.9
75.0
±
12.3 0.488
Height, cm
156.0
±
8.4 153.9
±
5.5 156.2
±
8.7 0.497
Weight, kg
54.7
±
10.5 51.9
±
7.6
55.1
±
10.7 0.442
BMI, kg/m
2
22.4
±
3.6 21.9
±
2.5
22.5
±
3.7 0.767
Smoking, current,
n
(%)
2 (2.6)
0 (0.0)
2 (2.9)
1.000
Hypertension,
n
(%)
59 (75.6)
7 (87.5)
52 (74.3)
0.671
Diabetes,
n
(%)
20 (25.6)
2 (25.0)
18 (25.7)
1.000
Dyslipidaemia,
n
(%)
9 (11.5)
0 (0.0)
9 (12.9)
0.586
Coronary artery
disease,
n
(%)
7 (9.0)
1 (12.5)
6 (8.6)
0.546
Atrial fibrillation,
n
(%)
2 (2.6)
0 (0.0)
2 (2.9)
1.000
Hospital stay, days
18.4
±
7.8 29.8
±
17.0
17.1
±
4.6 0.003
SBP, systolic blood pressure; DBP, diastolic blood pressure; BMI, body mass index.
Table 2. Laboratory tests and echocardiographic measurements
All
(
n
=
78)
Pulmonary
complications
(
n
=
8)
No
complications
(
n
=
70)
p
-value
Laboratory parameters
Haemoglobin, g/dl
11.4
±
1.8 10.3
±
1.7
11.5
±
1.8 0.091
Pro-BNP, pg/ml
1259.9
±
4468.7
2375.3
±
4237.1
1113.6
±
4511.1
0.851
BUN, mg/dl
20.2
±
9.0 22.7
±
7.4
19.9
±
9.1 0.205
Creatinine, mg/dl
1.1
±
0.7
1.1
±
0.2
1.1
±
0.7 0.178
eGFR, ml/min/1.73 m
2
60.1
±
22.8 52.8
±
8.3
60.9
±
23.8 0.140
CKMB, ng/ml
2.0
±
2.4
1.2
±
1.0
2.1
±
2.6 0.268
Troponin I, μg/l
0.1
±
0.2
0.0
±
0.1
0.1
±
0.2 0.922
CRP, mg/dl
2.9
±
5.0
5.6
±
7.9
2.6
±
4.6 0.161
D-dimer, ng/ml
10460.4
±
11500.1
19191.5
±
16257.0
9256.1
±
10304.5
0.023
Echocardiographic parameters
LVEF, %
61.6
±
5.9 59.9
±
9.9
61.8
±
5.3 0.953
RV FAC, %
39.9
±
8.2 37.0
±
13.3
40.2
±
7.5 0.442
RVs
′
, cm/s
14.3
±
3.6 13.5
±
3.7
14.4
±
3.6 0.313
TAPSE, mm
18.5
±
3.1 18.1
±
2.1
18.5
±
3.2 0.781
PASP, mmHg
36.0
±
12.6 40.2
±
17.7 35.4
±
11.9 0.705
Pro-BNP, pro-brain-type natriuretic peptide; BUN, blood urea nitrogen; CKMB,
creatine kinase MB; CRP, C-reactive protein; eGFR, estimated glomerular filtra-
tion rate; LVEF, left ventricular ejection fraction; RV, right ventricle; FAC, frac-
tional area change; RVs
′
, tissue Doppler-derived tricuspid lateral annular systolic
velocity; TAPSE, tricuspid annular plane systolic excursion; PASP, pulmonary
artery systolic pressure.
Table 4. Univariate and multivariate analysis of
RV GLS for predicting pulmonary complications
Univariate
Multivariate
OR
95% CI
OR
95% CI
RV GLS, %
1.17
1.007–1.369
2.09
1.047–4.151
Hospital stay, days
1.17
1.041–1.307
1.64
1.053–2.560
D-dimer, ng/ml
1.00
1.00–1.00
1.00
1.000–1.000
Haemoglobin, g/dl
0.65
0.412–1.036
0.24
0.060–0.965
CI, confidence interval; OR, odds ratio.
Table 3. RV strain analysis measurements
according to pulmonary complications
All (
n
=
78)
Pulmonary
complications
(
n
=
8)
No complications
(
n
=
70)
p
-value
RV GLS, % –16.66
±
5.93 –12.40
±
6.41
–17.14
±
5.72 0.036
Basal septal
–15.35
±
7.73 –14.63
±
11.33
–15.43
±
7.32 0.779
Mid-septal
–17.47
±
6.94 –15.88
±
10.91 –17.66
±
6.43 0.662
Apico-septal
–15.26
±
11.87 –3.38
±
12.98 –16.61
±
11.04 0.010
Basal lateral
–14.81
±
14.19 –10.13
±
11.47 –15.34
±
14.44 0.166
Mid-lateral
–15.78
±
10.66 –10.63
±
13.18 –16.37
±
10.28 0.121
Apico-lateral
–14.36
±
13.38 –4.5
±
18.87
–15.49
±
12.31 0.108
RV GLS, right ventricular global longitudinal strain.

















