CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 1, January/February 2020
12
AFRICA
Statistical analysis
Since the survey did not capture where individuals sought care,
this analysis was limited to the rural population to minimise the
possibility of cross-contamination (study participants residing
near one facility but receiving treatment from another facility).
Because of the sparse distribution of healthcare facilities in
rural areas, the likelihood of individuals seeking care from a
healthcare facility other than their locally assigned facility was
believed to be lower. The analysis was restricted to individuals
residing near seven intervention facilities located in rural areas
and the seven matched control facilities. Due to difficulties in
matching intervention and control facilities supported by the
same implementation partner, select rural intervention facilities
were matched to control facilities located in more urban areas.
At baseline and end point, statistical differences between the
intervention and control groups with regard to demographics
and lifestyle characteristics were evaluated using a
t
-test for
bimodal variables and a chi-squared test for outcomes with more
than two values. The impact of HHA intervention, defined as the
treatment effect (TE) on hypertension awareness and knowledge,
BP screening and patient recall of provider recommendation was
assessed using a difference-in-differences (D-in-D) regression
analysis, which minimises bias due to other factors that change
over the same time frame.
Results
A total of 838 individuals were surveyed at baseline (intervention,
n
=
432; control,
n
=
406) and 698 at the end point (intervention,
n
=
364; control,
n
=
334). Demographics (age, geographic location
and education) were well balanced between the intervention and
control groups sampled at baseline and the end point (Table 2).
Nevertheless, the two treatment groups at both baseline and end
point varied with regard to wealth and lifestyle characteristics.
At both baseline and end point, individuals in the intervention
group were wealthier and tended to consume one or more
servings of fruit per day (
p
<
0.05 for all). In addition, at the end
point, a significantly greater proportion of individuals in the
intervention group consumed alcohol and one or more servings
of vegetables per day (
p
<
0.05 for both).
Hypertension awareness (defined as having heard of
hypertension) among the intervention group was high at baseline
(91.0%) and increased to 94.9% by the end point (Table 3). In
contrast, hypertension awareness was much lower at baseline in
the control group (79.1%) but had increased to 96.7% by the end
point. Of note, the D-in-D method’s underlying assumption of
parallel trends could not hold for this outcome, as an increase of
17 percentage points (pp) from an initial level of 91.0% was not
feasible in the intervention group.
Family and friends were the primary source of information
on hypertension for both the intervention and control groups at
baseline and the control group at the end point. However, by the
end point, a healthcare provider or facility became the primary
source of information for individuals in the intervention group
(TE, 19.4 pp;
p
<
0.05; Table 3).
In general, the intervention group experienced an increase in
knowledge of individual risk factors for hypertension. Significant
improvement was observed in individuals’ knowledge of tobacco
use as a risk factor for hypertension with intervention (TE, 4.0
pp;
p
<
0.05; Table 3). Within 12 months, individuals’ knowledge
of three or more hypertension risk factors also showed a trend
toward improvement in the intervention group [TE, 3.8 pp;
p
=
not significant (NS)].
A positive improvement in individuals’ knowledge of
hypertension management was seen in the intervention group.
Identification of alcohol reduction as a method for managing
hypertension significantly increased four-fold in the intervention
group (TE, 8.4 pp;
p
<
0.01). In addition, positive trends were seen
in the proportion of individuals who identified salt reduction as
a method for hypertension management (TE, 1.0 pp;
p
=
NS)
in the intervention group. Individuals’ knowledge of three or
more or five or more methods for managing hypertension also
improved three-fold (TE, 3.7 pp;
p
=
NS) and 17-fold (TE, 1.7
pp;
p
=
NS), respectively, in the intervention group.
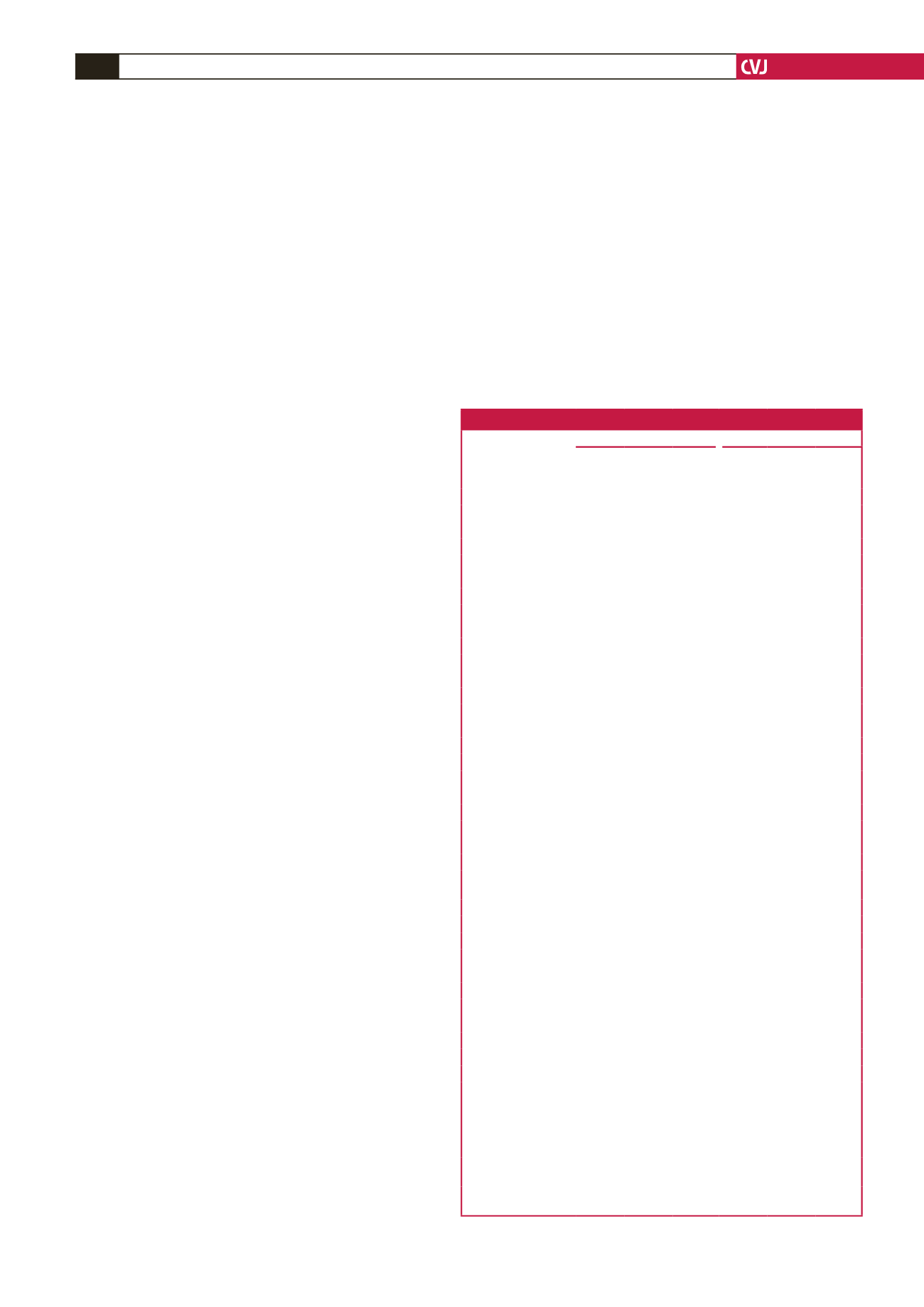
Table 2. Characteristics of survey respondents residing in rural areas
Baseline
End point
Interven-
tion
(
n
=
432)
Control
(
n
=
406)
p
-value
Interven-
tion
(
n
=
364)
Control
(
n
=
334)
p
-value
Geographic region, %
Central or eastern
63.6
63.6
0.345
75.0
72.4
0.175
Nairobi
0.0
0.0
0.0
0.0
Nyanza
10.1
0.0
9.8
0.0
Rift Valley
0.0
10.3
0.0
11.4
Western
26.4
26.1
15.3
16.2
Residence location, %
Rural
93.6
99.4
0.014*
69.3
99.5
0.000**
Urban
a
6.4
0.6
30.7
0.5
Age, years, %
18–24
18.7
20.0
0.647
22.4
14.3
0.128
25–29
12.7
8.9
14.2
16.0
30–34
10.9
12.3
14.0
10.8
35–39
11.2
13.3
9.3
7.6
40–44
11.2
8.7
11.6
9.7
45–49
6.6
6.9
7.0
8.8
≥
50
28.8
30.0
21.6
32.8
Gender, %
Male
48.7
46.0
0.269
50.6
55.7
0.448
Female
51.3
54.0
49.4
44.3
Education, %
Nursery/kindergarten 1.8
2.0
0.834
3.5
2.7
0.310
Primary
47.4
48.7
37.1
48.2
Post-primary,
vocational
4.1
3.5
4.3
5.3
Secondary, A-level
36.4
32.2
39.3
30.1
College (mid-level)
6.0
6.5
11.8
6.4
University
1.7
1.7
1.4
1.2
No school attended
2.5
4.8
2.5
6.0
Wealth quintile, shillings/month, %
≤ 653
34.3
33.5
0.000**
25.6
37.9
0.000**
654–2 158
17.2
13.6
22.4
20.6
2 159–2 633
25.8
51.6
15.4
38.8
2 634–3 631
21.2
0.5
32.4
1.0
≥
3 632
1.5
0.8
4.2
1.7
Lifestyle characteristics, %
Non-smoker
87.8
91.5 0.392
92.0
86.6 0.104
Does not drink
alcohol
78.0
82.8 0.177
80.2
87.4 0.023*
Consumes
≥
1 fruit
serving/day
52.0
26.3
0.001**
60.8
36.0
0.010*
Consumes
≥
1
vegetable serving/day
68.1
56.5
0.446
84.9
54.1
0.016*
*
p
<
0.05; **
p
<
0.01 vs control.
a
Select intervention facilities were matched to control facilities.



















