CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 1, January/February 2020
18
AFRICA
can be seen. With 10 mortalities among our cases, we compared
596 patients. The paired-samples
t
-test was performed between
these two groups and a statistically significant difference was
found (
p
<
0.01).
Discussion
In the treatment of coronary artery disease, which is one of
the major causes of death worldwide, CABG surgery plays
an important role. CABG surgeries are often performed with
CPB and most of the time this technique is the major part of
residency training.
6
CPB provides great support to the surgeon
during distal anastomoses and in the positioning of the heart.
Performing an anastomosis on the beating heart is one of
the biggest drawbacks in the OPCAB approach. However,
OPCAB is an important surgical technique that can be used for
prevention of the side effects of cannulation and CPB.
7
Although there are more than 100 randomised studies and 60
meta-analyses in which comparison of these two techniques were
made, there was no clear superiority of one technique over the
other. However the experience of the surgeon was emphasised
in all reports.
1
When chosen routinely, OPCAB surgery can be
as effective as on-pump bypass surgery.
8
In meta-analyses of
randomised studies, one to two years’ follow up of low-risk
patients showed similar mortality rates, myocardial infarction and
need for repeat revascularisation to on-pump surgery.
9,10
Experience
of the surgeons participating in the studies increased the success
of OPCAB and no significant difference was found between the
patients operated with on- and off-pump techniques.
5,11
The impact of the surgeon’s experience in OPCAB success
was most strikingly demonstrated in the ROOBY study.
12
The
five-year follow up of patients showed a clear superiority of
ONCAB over OPCAB (operated on by a minimum of 20
experienced OPCAB surgeons). In the light of these studies and
with our dedicated surgical team led by an experienced OPCAB
surgeon, OPCAB surgery has became our routine choice for
CABG operations.
In Table 2, the morbidities experienced in the postoperative
period are shown. We compared our postoperative atrial
fibrillation, intra-operative balloon pump (IABP) insertion,
cerebrovascular events and postoperative revision numbers with
those of the study by Taggart
et al
.
13
with 618 patients in the
OPCAB single mammary artery group, and those of the study
by Benedetto
et al
.
5
While the number of patients with IABP was
similar, the number of cerebrovascular events and revisions was
fewer in our study.
One of the major advantages of the OPCAB technique
compared to ONCAB is the reduced manipulation of large
vessels. During cannulation, embolisation of atheromatous
plaque from the aorta, bleeding, iatrogenic dissection and
end-organ malperfusion may develop. In addition, cross-
clamping can cause injury to the aorta, which can be avoided
with the OPCAB technique. However, the risk of CVI is not
reduced in OPCAB. The main reason for this is the side-clamp
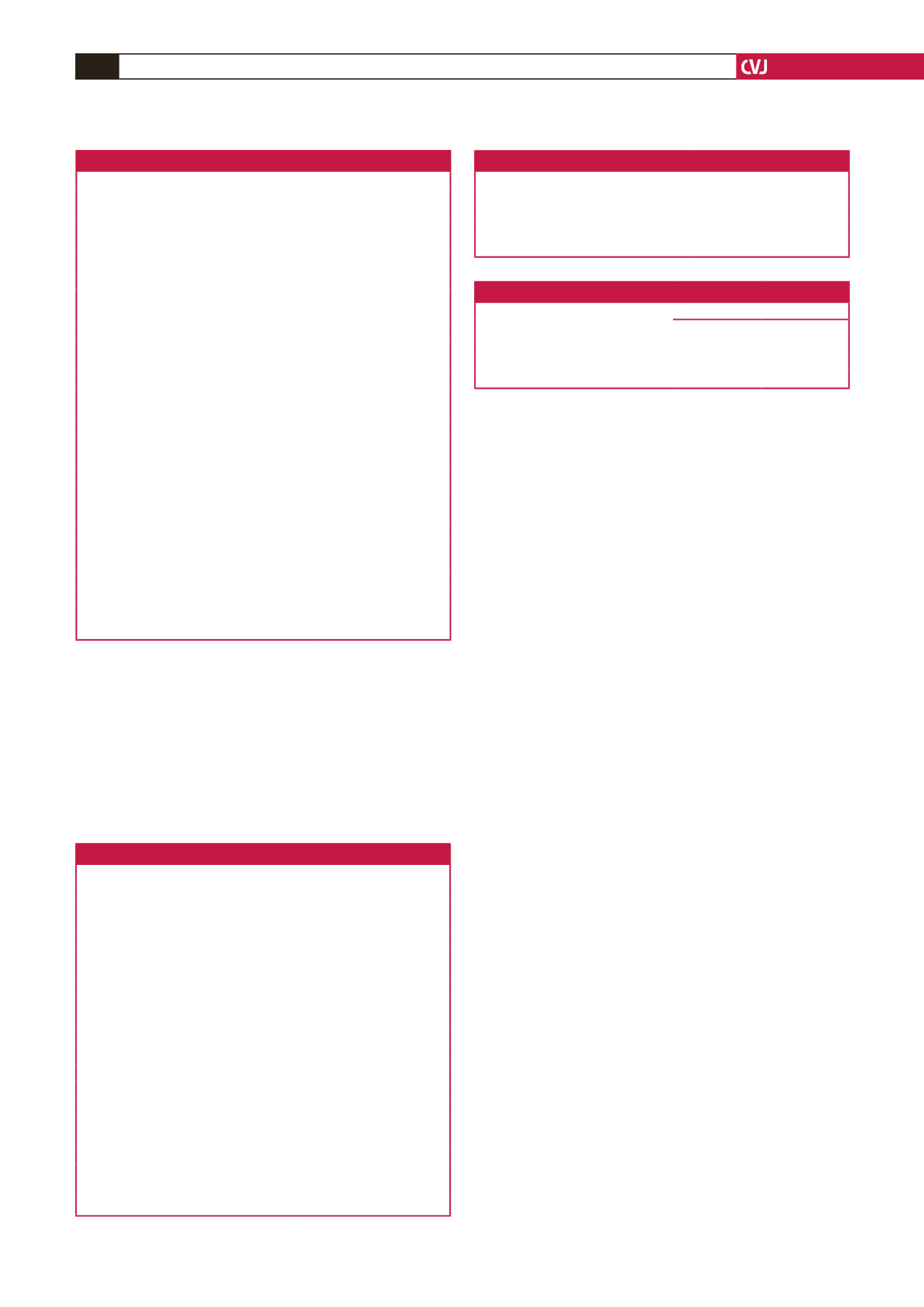
Table 1. Baseline characteristics of the patients
Variables
n
(%) or mean
±
SD
Female
132 (21.8)
Male
474 (78.2)
Age (years)
62.25
±
9.47
Body mass index (kg/m
2
)
29.58
±
4.98
Recent myocardial infarction
Yes
362 (59.7)
No
244 (40.3)
Diabetes mellitus
Yes
329 (54.3)
No
277 (45.7)
Hypertension
Yes
323 (53.3)
No
283 (46.7)
Chronic obstructive pulmonary disease
Yes
398 (65.7)
No
208 (34.3)
Smoking history
Yes
323 (53.3)
No
283 (46.7)
Renal disease
No renal disease
580 (95.7)
Dialysis dependent
6 (1)
Creatinine > 2.3 mg/dl
20 (3.3)
Ejection fraction
<
35%
61 (10.1)
35–50%
285 (47.0)
> 50%
260 (42.9)
Table 2. Postoperative findings
Variables
Mean (min–max) or
n
(%)
Intubation (hours)
6.31 (1–240)
ICU stay (days)
1.22 (0.04–18.75)
Hospital stay (days)
5.62 (3–48)
Intra-aortic balloon pump
Yes
29 (4.8)
No
577 (95.2)
Inotropes
None
489 (80.7)
Dopamine
84 (13.9)
Dopamine + noradrenaline
33 (5.4)
Drainage (ml), mean
±
SD
683.58
±
193.52
Revision
Yes
5 (0.8)
No
601 (99.2)
Postoperative atrial fibrillation
Yes
36 (5.9)
No
570 (94.1)
Cerebrovascular incident
Yes
2 (0.3)
No
604 (99.7)
Table 3. Number of distal anastomosis
Number of vessels
n
(%)
1 vessel
48 (7.9)
2 vessels
232 (38.3)
3 vessels
223 (36.8)
4 or more vessels
103 (17.0)
Table 4. Results of pre- and six-month postoperative LVEF comparison
Paired-samples statistics
Variable
Mean (
n
)
SD
Pre-operative
50.43 (593)
9.36
Postoperative
51.01 (593)
8.67
*
p
<
0.01.



















