CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 1, January/February 2020
14
AFRICA
Individuals’ knowledge of hypertension-related consequences
remained relatively unchanged. This was expected to a
certain extent, as the programme intervention did not educate
healthcare providers or the general public on the consequences
of hypertension.
7
In addition, HHA intervention areas did not
have a significant change in the number of individuals screened
for BP or diagnosed with hypertension, emphasising the need
for more innovative outreach activities/approaches to identify
individuals at high risk for hypertension, including those who
may not necessarily visit healthcare facilities.
To the best of our knowledge, this is the first study to
characterise and intervene to improve individuals’ awareness
and knowledge of hypertension among the rural population in
Kenya. Previous studies have reported a low degree of awareness
among Kenyans, but clinically meaningful comparisons were
not possible due to a lack of a standardised definition for
hypertension awareness.
2,5,6,11
However, a recent qualitative study based on a series of focus
group discussions with 53 individuals with HIV-1 conducted
at the Kenyatta National Referral and Teaching Hospital
Comprehensive Care Centre reported a gap between hypertension
awareness and knowledge, similar to what was seen in this study.
11
Respondents commonly referred to hypertension as ‘pressure’
and, although all of the participants had heard of the term,
most were unable to adequately describe it. Stress followed by
fatty foods, excessive salt intake, and physical inactivity were the
most frequently cited causes of hypertension. All respondents
demonstrated some knowledge regarding treatment modalities
for hypertension; however, most believed that hypertension could
not be prevented.
This gap between awareness and knowledge/understanding is
not strictly limited to hypertension and extends to individuals’
awareness and understanding of CVDs. A systematic review
evaluating awareness and knowledge of CVDs in sub-Saharan
Africa found that awareness, when reported, was high; however,
knowledge and understanding of CVDs and CVD risk factors
were poor.
12
Although limited, the data suggest that individuals
may benefit from intervention efforts designed to not only
raise awareness but also improve general understanding and
knowledge of hypertension. The HHA programme’s positive
impact on knowledge of hypertension may help to address
this critical gap in communication, and, when coupled with
the previously reported facility-level improvements in provider
education and ability to diagnose and treat hypertension,
7
may
lead to greater utilisation of hypertension services and, in turn,
timely diagnosis and treatment of hypertension.
There are some inherent limitations associated with this
analysis. The generalisability of the data is limited, in part, by
study design. This study was not designed to collect nationally
representative findings and therefore data interpretation is
limited to individuals residing near the study sites. In addition,
this study did not capture where respondents received care.
Potential ramifications of receiving care at distant sites were
mitigated by focusing on the rural population, which, due to
limited access to healthcare facilities, is more likely to receive
care at the local facility. The study design did not the capture
frequency and type of study- and non-study-related hypertension
awareness/education events conducted within the study area,
which may affect programme evaluation.
Furthermore, the short duration of this study may not be
sufficient for evaluating the impact of the HHA programme,
as significant changes in individuals’ behaviours and attitudes
towards hypertension care may require a longer period of
time in this setting. The impact of the HHA programme may
be underestimated as HHA-trained healthcare providers from
intervention facilities may have been moved and replaced with
untrained healthcare providers, a by-product of routine transfer
and the devolution of the Kenyan government,
8
which occurred
during the 12-month study period.
Conclusion
Little is known about how to rapidly improve control of
hypertension in low- to moderate-income countries. The results
from this study may help to develop more realistic expectations
on the anticipated rate of improvement in individuals’ awareness
and knowledge of hypertension and health-seeking behaviour
towards hypertension care. In this study, individuals residing
in rural Kenya demonstrated a high degree of hypertension
awareness; however, their medical knowledge of hypertension
was quite poor.
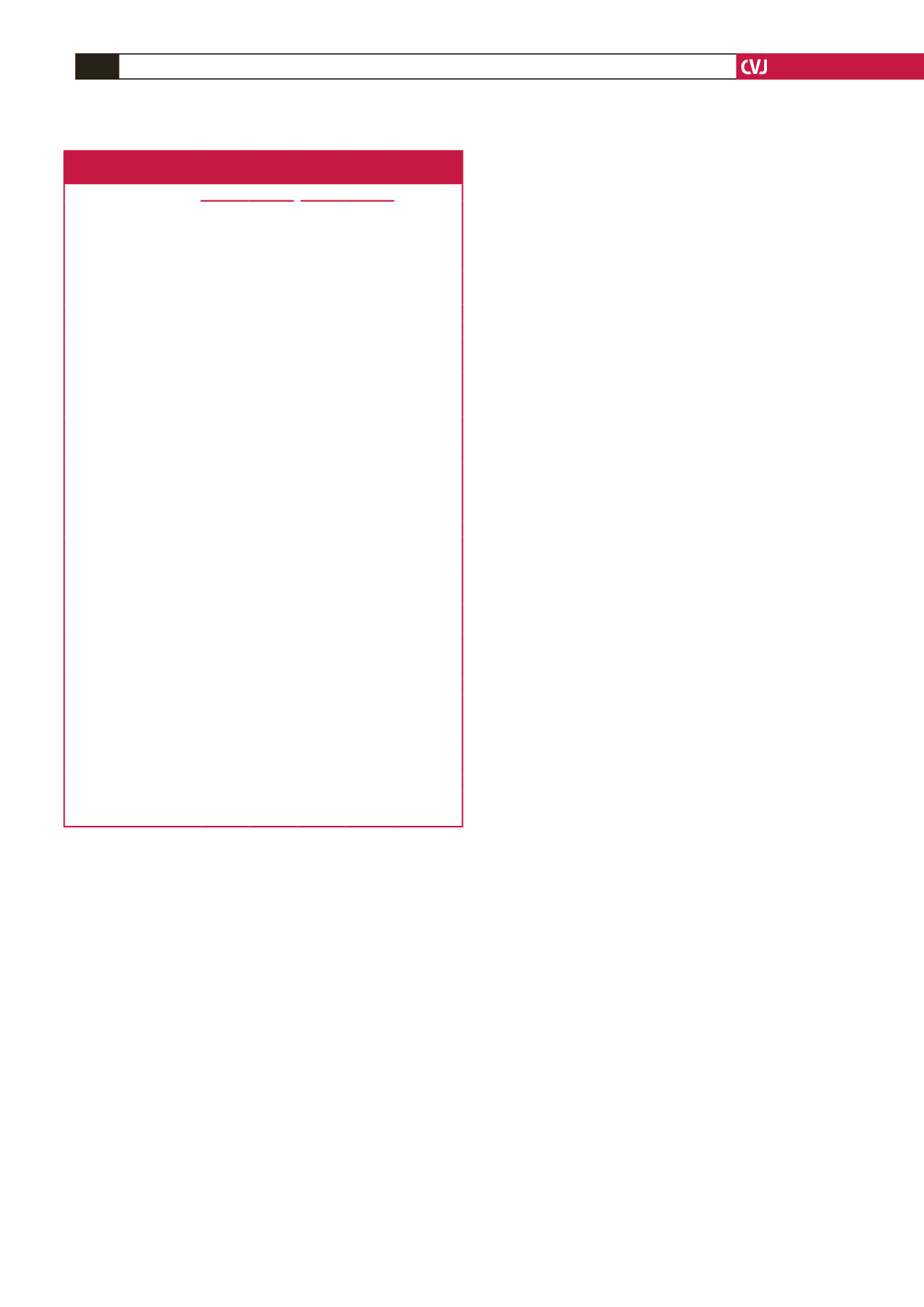
Table 4. Impact of Healthy Heart Africa on hypertension diagnosis and
provider’s recommendation
Baseline
End point
Treatment
effect (SE),
percentage
point
Interven-
tion
(
n
=
432)
Control
(
n
=
406)
Interven-
tion
(
n
=
364)
Control
(
n
=
334)
Individuals who reported
being screened for BP, % 74.3
62.6
72.9
77.6 –19.9 (7.8)*
Last time BP screening was performed, %
≤ 6 months
38.7
24.4
37.8
39.4 –15.2 (4.6)**
7–12 months
10.2
8.8
12.1
16.3
7.2 (4.8)
≥
12 months
24.8
27.8
22.2
21.9
0.7 (4.1)
BP screening location, %
Public hospital
29.3
29.0
27.1
19.9
8.3 (7.8)
Public health centre or
dispensary
40.9
24.1
35.9
44.6 –16.2 (9.0)
Private hospital
5.6
8.9
13.3
18.2 –2.7 (3.4)
Private health centre or
dispensary
11.3
6.1
15.5
13.7 –4.6 (6.4)
At screening event
1.2
0.8
2.5
8.1 –7.4 (2.9)
Other
7.7
10.4
15.0
21.1 –2.0 (1.6)
Individuals who reported
being diagnosed with
hypertension, %
14.9
8.8
12.9
10.3 –0.03 (3.3)
Timing of hypertension diagnosis, %
≤ 6 months
3.8
2.9
2.7
2.9 –1.2 (3.0)
7–12 months
2.1
1.0
3.8
1.3
2.5 (1.1)
>
12 months
8.8
4.9
5.5
5.1 –1.3 (2.7)
Individuals’ recall of healthcare providers’ recommendation, %
≥
1 healthcare providers’
recommendation
13.4
8.8
9.8
9.3 –2.3 (3.5)
≥
3 healthcare providers’
recommendations
0.1
2.1
0.5
1.4
1.2 (0.9)
Medication
13.1
7.1
7.2
8.2 –5.0 (2.5)
Reduction in salt
2.2
3.8
4.0
4.0
2.0 (1.6)
Lose weight
0.1
2.0
0.6
1.3
1.9 (1.7)
Reduce alcohol consump-
tion
0.2
0.7
0.6
0.0
1.3 (0.5)*
Exercise
1.4
2.3
1.3
1.3
1.3 (1.5)
Reduce stress
3.5
2.1
3.8
3.6
0.4 (1.3)
Home remedies
0.3
0.9
0.1
0.7
0.3 (0.7)
Unable to recall
0.9
0.1
1.6
0.6
0.8 (1.5)
*
p
<
0.05; **
p
<
0.01 vs control. BP: blood pressure; SE: standard error.



















