CARDIOVASCULAR JOURNAL OF AFRICA • Vol 21, No 3, May/June 2010
156
AFRICA
tricuspid insufficiency, ejection fraction of 40 to 45% and 36
mmHg pulmonary artery pressure. No thrombus was detected
in any cavity.
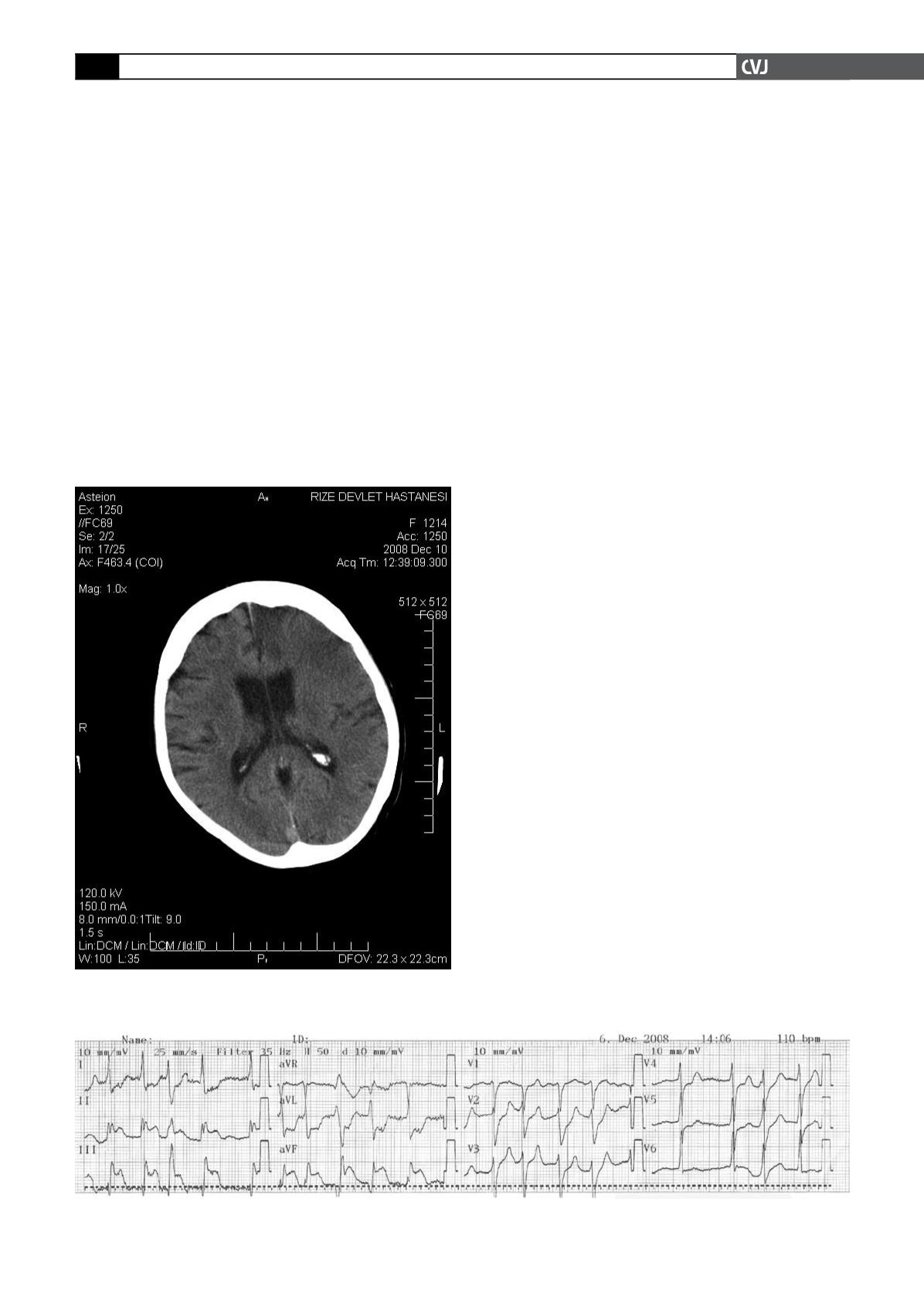
The patient had deteriorated after two hours of intravenous
TT. Motor aphasia and right hemiparesis then developed. The
Babinski sign was positive in the right lower extremity. Immediate
cerebral tomography (CT) was performed and showed no patho-
logical abnormality. The patient then consulted a neurologist. In
the second CT 12 hours later, extensive infarction of the left fron-
tal area was seen (Fig. 2). On the follow up, neurological deficits
had increased, congestive heart failure developed, and finally the
patient died on the ninth day following TT.
Discussion
STEMI is an urgent condition caused by acute thrombotic occlu-
sion of the coronary arteries. Angiographic studies have shown
that coronary arterial thrombosis is present in about 85% of
patients with STEMI.
6
The most important therapeutic method is
immediate recanalisation of the infarct-related coronary artery.
There are two methods to do this, PCI or a pharmacological
approach.
PCI is the more favourable approach, but it presents many
technical and scientific limitations. In our case, because of the
respiratory insufficiency, the patient could not lie down so we
could not do PCI. We decided to carry out intravenous TT with
streptokinase because of its lower incidence of cerebral haemor-
rhage.
TT is an effective and easy therapeutic method that can be
used anywhere and at any time. As in all therapeutic options,
TT has certain limitations and complications. The most impor-
tant and feared complication of a fibrinolytic agent is bleeding,
especially intracranial bleeding. It occurs in 0.9% of patients
treated with tPA.
5
Bleeding after fibrinolytic treatment is due
to the depletion of clotting factors and lysis of recently formed
haemostatic plugs.
7
TT for STEMI has reduced mortality at the expense of
additional intracranial haemorrhage. The proof of efficacy of
thrombolysis for STEMI comes from nine randomised placebo-
controlled trials in a total of 58 511 patients. The meta-analysis
of these trials showed an overall survival advantage of about 2%
(11.5 vs 9.6%) in favour of thrombolysis.
7
A meta-analysis of
randomised trials comparing PCI with thrombolytics for STEMI
at high-volume hospitals suggested that PCI improved 30-day
survival free of reinfarction (11.9 vs 7.2%). Stroke risk was also
reduced with PCI compared with thrombolytic therapy.
8
Two randomised trials compared low-molecular weight
heparin (LMWH), enoxaparin, with unfractionated heparin in
patients with UA or non-STEMI.
9,10
All patients received aspirin.
In both studies, there were reductions in short-term outcomes
of death, myocardial infarction (MI) and recurrent angina in
patients randomised to LMWH. A combined analysis of these
two trials showed significant 20% reductions in the short-term
risk of death and non-fatal MI in patients randomised to LMWH.
Randomised trials in STEMI patients conducted in the pre-fibrin-
olytic era showed that the risk of pulmonary embolism, stroke
and re-infarction was reduced in patients who received intrave-
nous heparin, providing support for the prescription of heparin to
STEMI patients not treated with fibrinolytic therapy.
With the introduction of fibrinolytic therapy and, importantly,
after the publication of the ISIS-2 trial,
3
the situation became
more complicated because of strong evidence of a substan-
tial mortality reduction with aspirin alone, and confusing and
conflicting data regarding the risk–benefit ratio of heparin used
as an adjunct to aspirin or in combination with aspirin and a
fibrinolytic agent. For every 1 000 patients treated with heparin
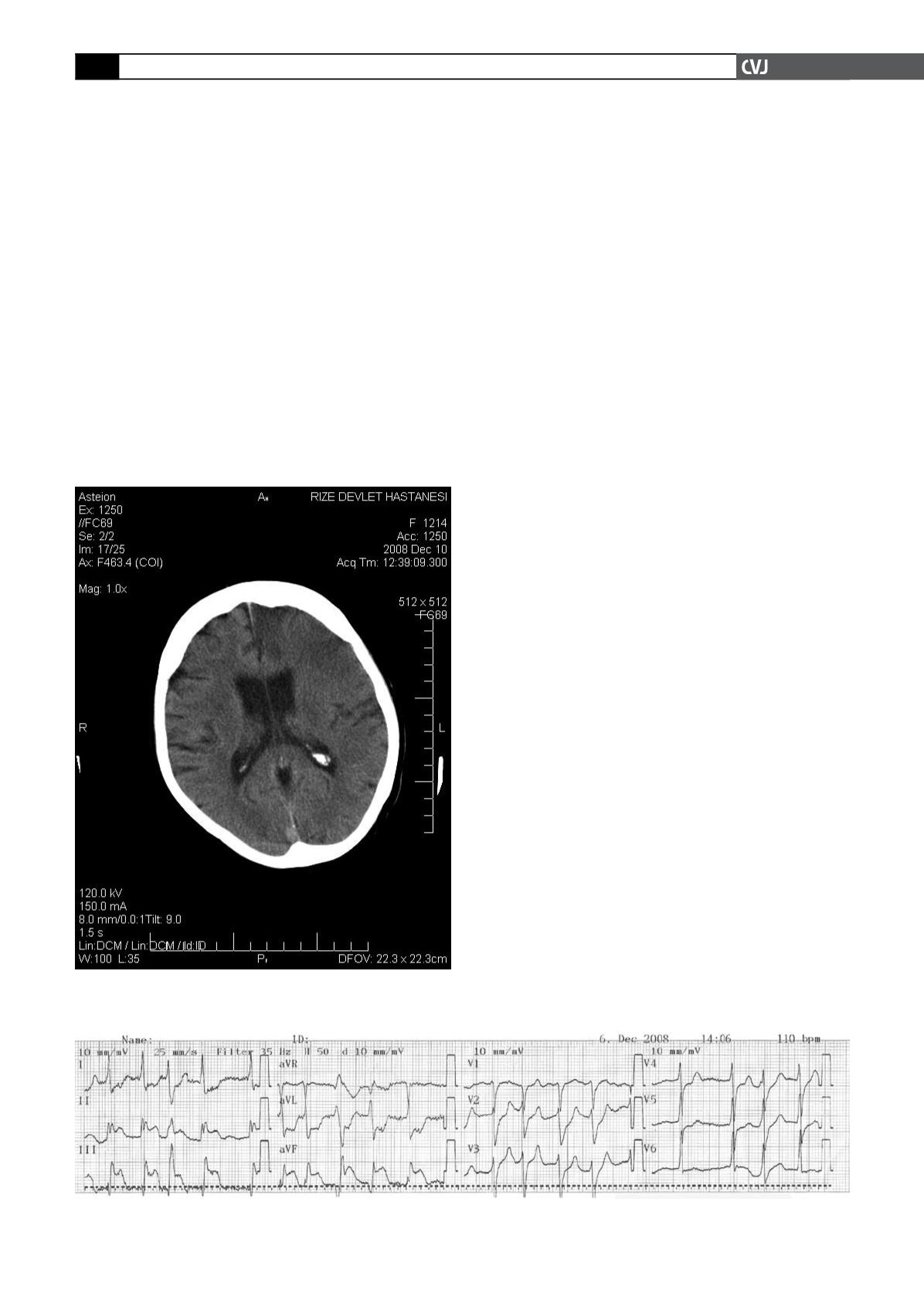
Fig. 1. Electrocardiography showing atrial fibrillation and
ST-segment elevation in leads D2, D3 and AVF.
Fig. 2. The second CT, 12 hours later, showing extensive infarction of the left frontal area.