CARDIOVASCULAR JOURNAL OF AFRICA • Vol 21, No 3, May/June 2010
AFRICA
159
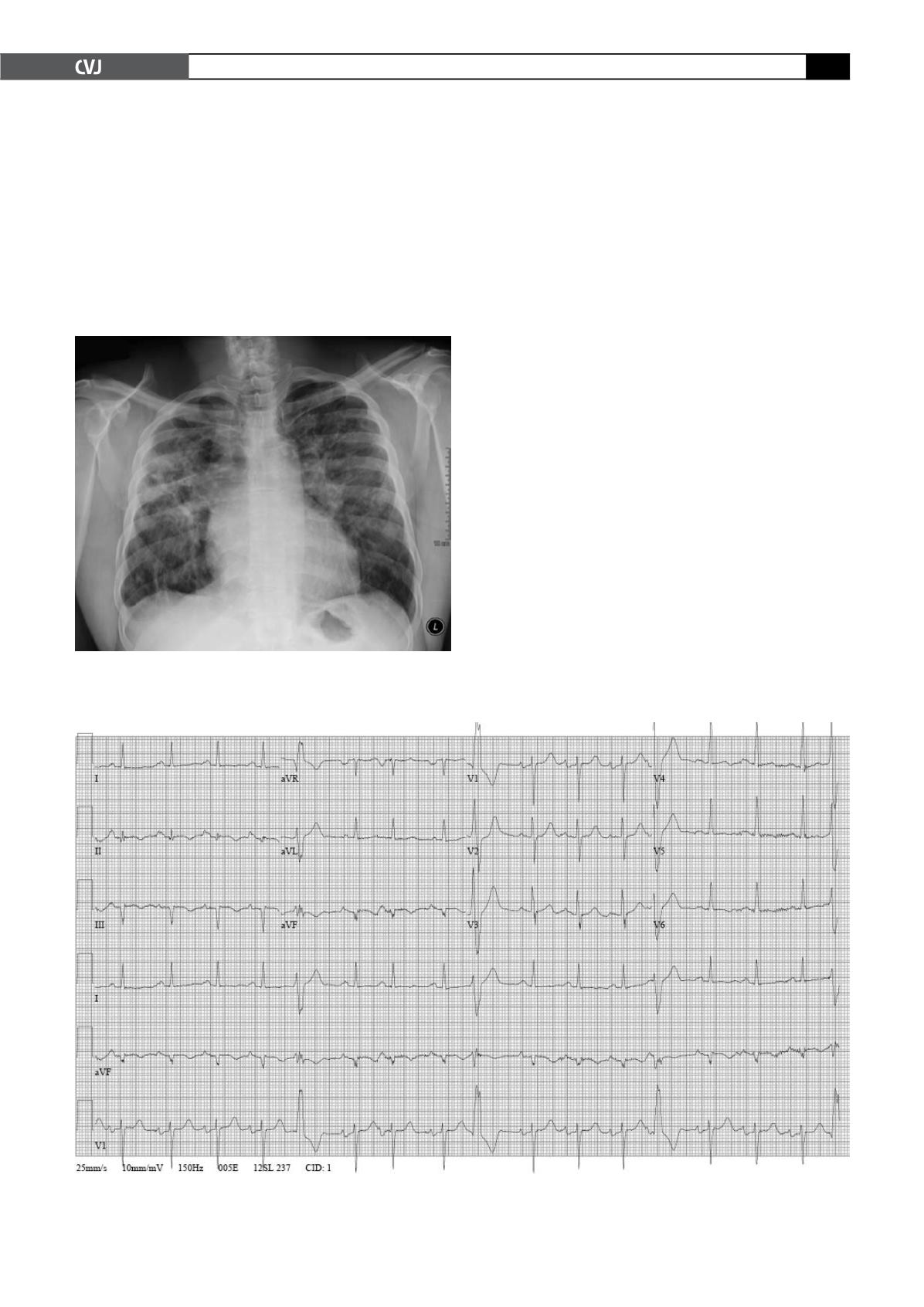
ECG revealed normal sinus rhythm with several pre-ventricular
contractions (PVCs) with right bundle branch morphologies
(most likely sub-aortic valve, left ventricular outflow tract in
origin),
12
a ventricular rate of 100 beats/minute, non-specific
atrio-ventricular delay, biatrial enlargement, and Q waves in
leads II, III and aVF with inverted T waves (Fig. 2).
Laboratory evaluation was significant for mildly elevated
AST at 151 U/l (normal
<
46 U/l) and ALT at 70 U/l (normal
<
53 U/l), LDH elevated at 438 U/l (normal
<
260 U/l), and
natriuretic peptide assay elevated at 460 pg/ml (normal
<
100 pg/
ml). White blood cell count, haemoglobin and differential were
all normal. Electrolytes including BUN and creatinine were also
normal.
Overnight the patient required intubation for hypoxaemic
respiratory failure. A bronchoscopy was performed which
revealed bloody transudate. No infectious organism was identi-
fied in the blood or respiratory secretions, including fungus,
acid-fast bacillus, Coccidiomycosis by serology or
Pneumocystis
carinii
by direct fluorescent antibody. HIV 1 and 2 serology was
negative.
A transthoracic two-dimensional echocardiogram revealed
a dilated left ventricle with severe global left ventricular hypo-
kinesis and an ejection fraction of 21%, without evidence of
increased echogenicity compatible with infiltrative disease or
fibrosis. E/E
′
was not significantly elevated (12.7), pulmonary
vein flow was diastolic-predominant and E/A was consistent
with pseudo-normalisation (left ventricular diastolic dysfunc-
tion). There was moderate to severe mitral regurgitation, which
was eccentric and posteriorly directed. Pulmonary artery systolic
pressure was estimated at 19 mmHg; the inaccuracy of this esti-
mate may have been due to positive-pressure ventilation, intrin-
sic lung disease, poor right ventricular function or inaccurate
Doppler of the tricuspid regurgitation.
A high-resolution CT scan of the chest was performed which
showed extensive bilateral parenchymal ground-glass opaci-
ties as well as focal areas of consolidation, bilateral hilar and
mediastinal lymphadenopathy and multiple pulmonary nodules.
Angiotensin converting enzyme level was 42 U/l (normal range
9–67 U/l).
Natriuretic peptide assay increased to 1 560 pg/ml. The
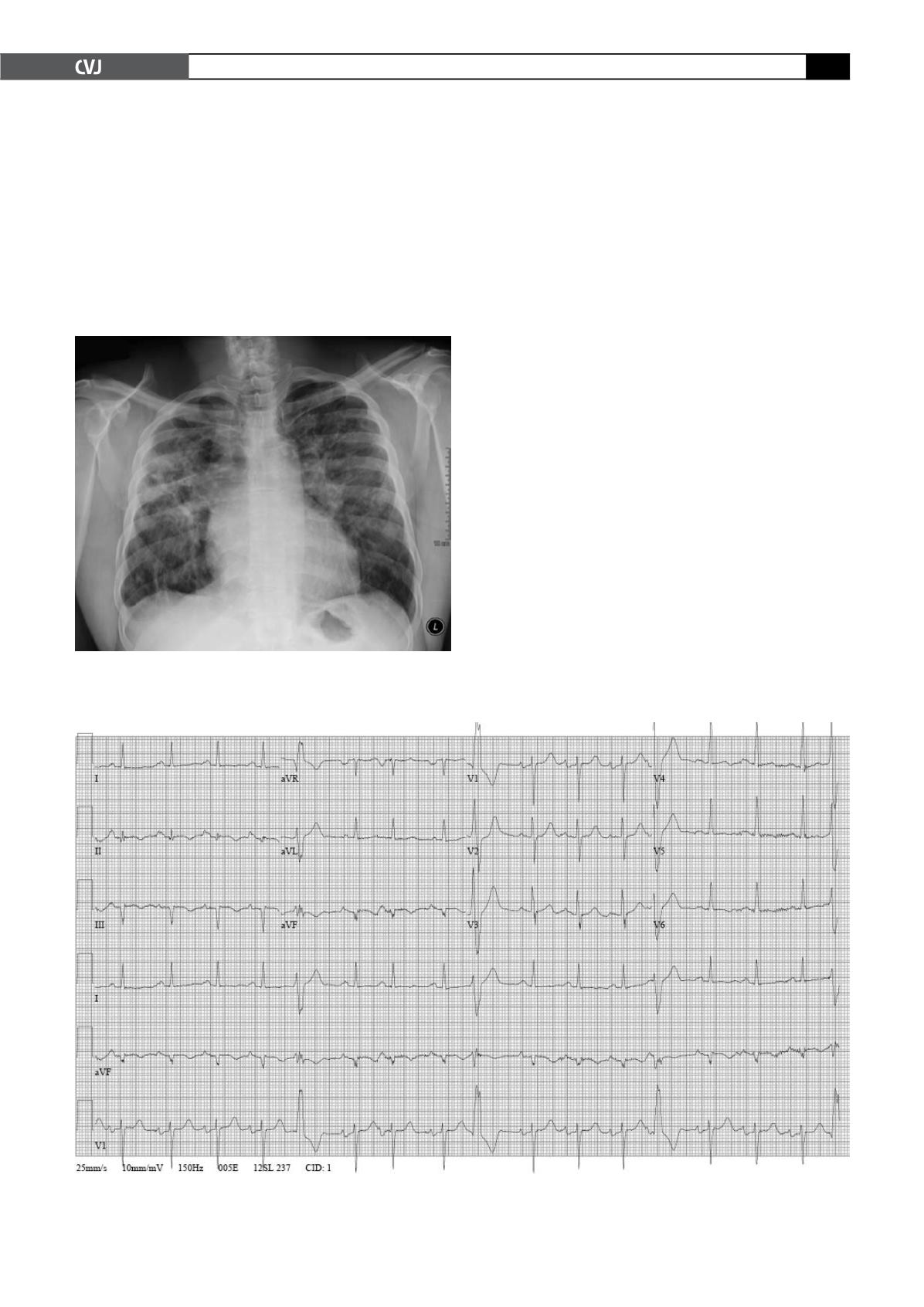
Fig. 1. Plain film of the chest demonstrating extensive
interstitial lung disease and peri-hilar consolidations
versus increased pulmonary vasculature.
Fig. 2. ECG demonstrating frequent PVCs (left ventricular in origin), non-specific atrio-ventricular delay, biatrial
enlargement and evidence of an old inferior infarct.