CARDIOVASCULAR JOURNAL OF AFRICA • Vol 21, No 4, July/August 2010
AFRICA
229
Coeur en sabot
F AZIZ, M ABED
Summary
In tetralogy of Fallot (TOF), the most common form of
cyanotic congenital heart disease, only a few patients reach
adulthood without surgical correction.We present a case of a
woman with TOF who was diagnosed at the age of 39 when
she presented with features of congestive heart failure. The
main factor contributing to her longevity included the slow
development of her pulmonary artery stenosis together with
left ventricular hypertrophy. Less than 3% of all patients
with uncorrected TOF survive beyond their 40s but late
operative repair is still a valuable option. This case provides
an insight into the late outcome of an older patient with
uncorrected TOF.
Keywords:
uncorrected TOF, congestive heart failure, longevity
Submitted 1/12/09, accepted 10/3/10
Cardiovasc J Afr
2010;
21
: 229–231
DOI: CVJ-21.010
More than 40 years have passed since the first successful repair
of tetralogy of Fallot (TOF), and currently, excellent results for
the repair of most TOF variants have been achieved. Although
most patients undergo radical repair during infancy and child-
hood, patients remaining undiagnosed and untreated until adult-
hood can still be treated. These patients have either a previous
palliative or natural collateral circulation to the lung or a mild
form of right ventricular outflow tract (RVOT) obstruction. A
few case reports of patients with TOF surviving until their eighth
decade of life have been reported.
1
The survival data of patients with TOF who have died without
surgical treatment reveal that 66% lived to the first year of life,
56% to two years, 49% to three years, and 25% to 10 years of
age. Thereafter, the hazard function (or the instantaneous risk of
death at any given age) remains essentially constant at 6.4% per
year, so that only 3% of persons born with TOF are alive at 40
years of age. The natural history of the disease is influenced by
the severity of the anatomical defect, primarily the severity of the
pulmonary stenosis.
2
Case report
A 39-year-old female patient was admitted to our hospital with
dyspnoea as the main symptom. She had had a murmur since
childhood but it was never investigated, and she was not able to
play as a child due to dyspnoea. Her dyspnoea had increased in
the previous two weeks, as had her generalised body oedema.
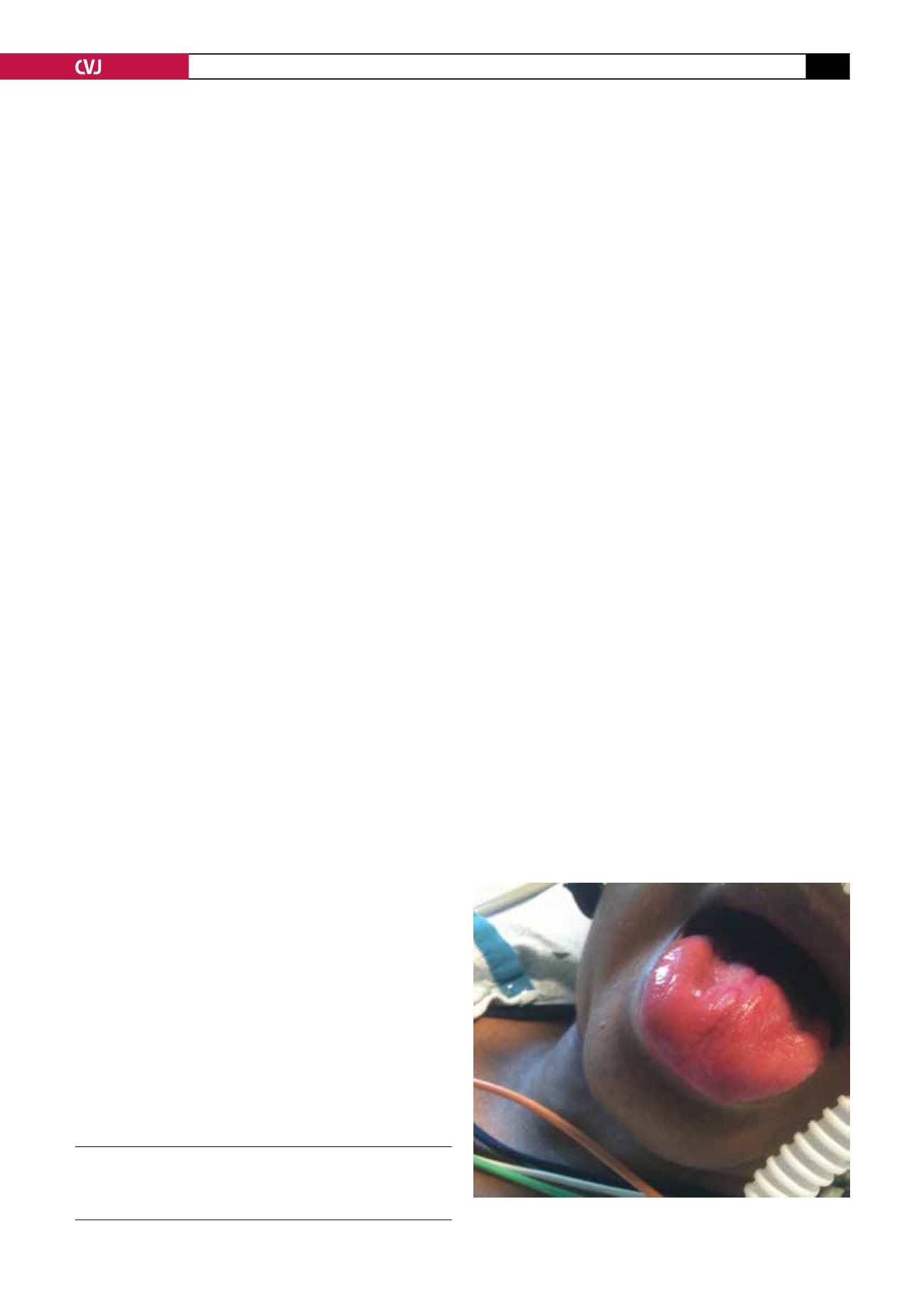
On physical examination, she was found to have blood pres-
sure of 90/60 mmHg with a regular heart rate of 66 beats per
min. Her jugular vein distention was raised about 15 cm above
the sternal angle with a prominent A wave. She had central and
peripheral cyanosis (Fig. 1). The pericardial examination was
significant for the visible apex beat pulsations in the fifth inter-
costal space in the mid-axillary line and there were also visible
pulsations along the parasternal border and second intercostal
space. The apex beat was palpable in the fifth intercostal space
with ill-sustained heave. The second heart sound was palpable in
the second intercostal space.
Auscaltation of the heart revealed S1, S2 and S4 along with
a systolic murmur of grade 4/6 with maximum intensity in the
left second intercostal space. Lung auscultation revealed bilateral
crackles up to one-third of the chest bilaterally. The abdominal
examination was significant for tender hepatomegaly, which
was four fingers below the costal margins, and the total hepatic
span was measured to be 19 cm. She had bilateral pedal oedema
extending up to the lower abdomen and involving the external
genitalia (Figs 2, 3). She also had grade II clubbing bilaterally.
The chest X-ray showed a large boot-shaped heart (Figs 4–6).
The patient was admitted to the critical care unit with a diagnosis
of congestive heart failure and she was started on empirical ther-
apy. The next day an echocardiogram was done, which showed
marked left ventricular hypertrophy, a dilated left and right
atrium and severe tricuspird regurgitation associated with severe
pulmonary artery stenosis, ventricular septal defect (VSD) and
moderate to severe right ventricular hypertrophy. On the basis of
these findings, a diagnosis of tetrology of Fallot was made and
the patient was referred for corrective surgery.
Discussion
The unusual longevity in some cases of tetralogy of Fallot is
probably related to comparatively favorable anatomical abnor-
malities. Higgins,
3
after reviewing the literature, concluded that
longevity is determined predominantly by the early development
Department of Internal Medicine, MSSM, Jersey City
Campus, New Jersey, USA
FAHAD AZIZ, MD,
MARY ABED, MD
Fig. 1. Central cyanosis.