CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 10, November 2012
e8
AFRICA
vascular obstruction. The results showed patent bilateral femoral
and popliteal arteries with normal compressibility.
The patient was transferred to the intensive care unit of
cardiovascular surgery. During her follow up, the increased blood
pressure was unresponsive to high-dose combined parenteral
antihypertensive therapy (10 µg/kg/min nitroprusside plus 10
µg/kg/min esmolol). The patient’s pain had not subsided and had
even increased after her admission.
The patient and her family were informed about the condition
and the risk of aortic rupture. A written informed consent was
obtained and a cesarean section was performed 12 hours after
her admission, in order to protect both mother and foetus from
the catastrophic consequences of aortic rupture and to control
the patient’s pain and severely increased blood pressure. A male
foetus weighing 1.45 kg was delivered.
On postoperative follow up, the blood pressure had lowered
and the pain had subsided. On postoperative day 3, repeated
thoraco-abdominal CT scans showed stability of the pre-existing
dissection line. The pulselessness in the patient’s left leg had also
recovered after the delivery. Conservative management of the
patient was therefore decided on.
A blood test for karyotyping was made in order to exclude the
diagnosis of Turner syndrome and a 46 XX normal karyotype
was obtained. The patient has maintained good general condition
and cardiovascular function four months postoperatively and to
date.
Discussion
It is well known that during the third trimester, there are maximal
increases in stroke volume, heart rate and cardiac output, and
in left ventricular wall mass and end-diastolic dimensions. In
addition, oestrogen reportedly inhibits collagen and elastin
deposition in the aorta, while progestogen accelerates deposition
of non-collagen proteins in the aorta.
5
These hormonal effects
lead to a fragmentation of the reticulin fibers, diminished
concentration of acid mucopolysaccharides, and loss of the
normal corrugation of the elastic fibers.
6
These haemodynamic changes occur in every pregnancy
and it is hypothesised that aortic dissection may have some
aetiological factors, such as an inborn defect in the arterial
wall.
1,2
Most of the reported cases had some predisposing risk
factors, including Marfan syndrome, Turner syndrome and
congenital heart diseases. In the present case, however, none of
the above risk factors were present and acute dissection of the
aorta developed spontaneously.
Although the clinical presentations of AAD are well defined,
the diagnosis is often overlooked. A study evaluating the
clinico-pathological features of patients with aortic dissection
over a 27-year period shows that misdiagnosis occurred in 85%
of patients presenting with acute dissection.
6
This interesting
finding has been confirmed by a number of case reports in
which the diagnosis was initially missed during pregnancy and
the peripartum period.
2,7,8
Although suggested by the clinical findings, a reliable
diagnosis of aortic dissection must be confirmed by specific
imaging methods, including echocardiography, contrast-
enhanced CT, aortography and magnetic resonance imaging.
Transthoracic echocardiography was suggested for the initial
screening of patients with suspected aortic dissection.
6
Although
the sensitivity and specificity can be up to 75 and 90%,
respectively, in type A dissections, the diagnostic value of this
procedure is of limited value in the case of type B dissections.
Our presenting patient’s symptoms and examination findings
were suggestive of aortic dissection. A rapid diagnosis was made
within 12 hours after her admission by thoraco-abdomianl CT
scan.
Aortic dissections are divided into two types according to
the Stanford classification system: type A always involves the
ascending aorta, while type B begins in the descending aorta
distal to the left subclavian artery.
4
In the International Registry
of Acute Aortic Dissection (IRAD), 62% of dissections are type
A and 38% are type B.
9
Patients with type B dissections tend to be older, heavy
smokers with chronic lung diseases, and more often have
generalised atherosclerosis and hypertension, compared with
patients who have proximal aortic dissections. The diagnosis of
acute type B dissection in pregnancy is rare.
10
A high incidence of foetal intra-uterine demise or subsequent
neonatal fatality has been linked to type B dissections.
9
In
the presenting case, however, early delivery of the foetus and
medical management of the mother were adequte to save both
mother and baby’s life.
The treatment of type B dissections is medical, with close
follow up of high blood pressure. Surgical treatment should
be reserved for patients who have persistent pain, uncontrolled
hypertension, occlusion of a major arterial trunk, frank aortic
leaking or rupture, or development of a localised aneurysm.
6,9
Similarly, in the present case, a primary caesarean section
followed by conservative management of the dissection was the
treatment of choice. Nevertheless, patients with uncomplicated
distal dissections treated for blood pressure control have an
in-hospital mortality of 10%.
6,10
The priority indication for termination of pregnancy in this
case was aimed at sparing the lives of both the mother and foetus,
since the elimination of the negative impact of pregnancy-related
haemodynamic changes on the AAD enhanced the chance of
maternal and foetal survival. Our approach to the present case
was consistent with data described in the literature, in which the
best survival rates (mother and foetus) are based on gestational
age.
7-10
Therefore, if the dissection presents after 32 weeks, when
the foetus has viability, pregnancy termination with or without
surgical repair should be performed.
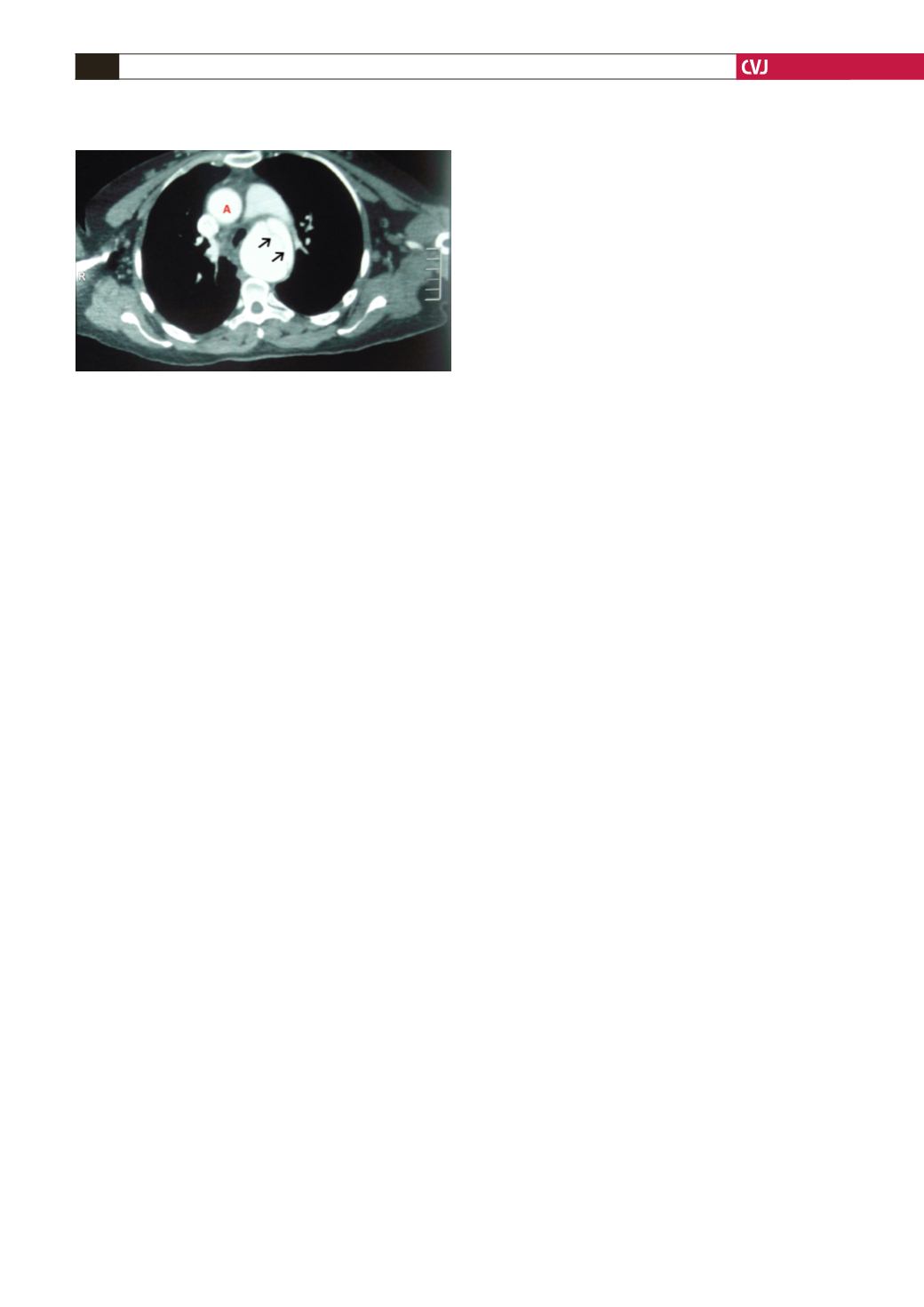
Fig. 1. Contrast-enhanced CT scan obtained after admis-
sion revealed the normal appearance of the ascending
aorta (A). The arrows indicate a large dissection line in
the descending aorta distal to the left subclavian artery
(
type B).