CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 10, November 2012
AFRICA
e3
than 10% whatever the form.
6
In our study, the incidence was
5.6%.
This frequency distribution is due to the heterogeneity in
definitions of pacemaker infection.
The factors predisposing to the occurrence of infection after
implantation of a pacemaker are diabetes, cancer, long-term
treatment with corticosteroids or anticoagulants, the presence
of postoperative haematoma, surgeon’s inexperience, and the
number of times the operation is repeated.
7,8
Other factors were
also implicated, such as the implantation of more than two
wires,
9
fever occurring within 24 hours of implantation, using a
temporary pacemaker, early re-operation,
10
and the placement of
the pacemaker box in the abdomen.
11
In our study, the risk factors found were: diabetes, dermatosis,
the long duration of pre-operative stay, the use of temporary
pacing, the number of people concurrently in the ward (between
four and five, average 4.5), postoperative haematoma and
repeating the operative procedure.
The mechanisms of infection were contamination of the
surgical site at the time of implantation
12
or haematogenous
spread from a remote focus, identified or not.
13
The average time
of onset of symptoms varied, according to the authors, between
six and 34.5 months.
14,15
We found the average time of onset to be
6.6
months in our study.
The clinical signs of infection of pacemaker varied according
to the location of the infected portion, from only localised signs
of a sagging in the pocket in about 70% of cases, local and
general signs in 20% of cases, to general symptoms in 10% of
cases.
16
The clinical presentation of infective endocarditis with a
pacemaker is right heart endocarditis with fever and pulmonary
symptoms secondary to septic emboli. None of our patients
showed signs of endocarditis but all had local signs of infection.
The microbiological diagnosis relies on sample collection
from a potentially infected site, repeated blood cultures, and
samples of different pre-operative implanted parts. In all patients,
a sample from the site of the pacemaker pouch was collected.
Staphylococcus
,
mostly coagulase negative, was involved in
50
to 90% of cases.
3
We found
Staphylococcus
in 80% of
cases, namely
Staphylococcus aureus
(40%)
and
Staphylococcus
epidermidis
(40%).
Moreover, mixed infections are not
uncommon. There can be associations of a staphylococcus with
other bacteria or fungi, or a combination of two different strains
of staphylococci.
17
The strong presence of skin bacteria is an
additional argument in favour of contamination during handling
of the pacemaker.
Echocardiography is the key to the morphological diagnosis
of endocarditis on pacemaker leads by visualising the
vegetations. Different morphologies of vegetations have been
described: floating ribbons, large rounded lesions, more or less
pedunculated, multilobed vegetations, and a sleeve around the
lead.
3
The sensitivity of transoesophageal echocardiography in
detecting vegetations is above 90% while that of transthoracic
echocardiography is above 30%.
13
In our study, no patient
received transoesophageal echocardiography. This would explain
the fact that we did not see any vegetations.
The management of pacemaker infection is difficult and has
been the subject of several studies. In infective endocarditis
secondary to pacemaker leads, all authors agree that removing
the implanted material is necessary for treatment.
18
On the other
hand, in local infections, opinions on how to treat are divided.
Some advocate conservative treatment
19
while others suggest
radical treatment.
17
However, current recommendations call for a
complete removal of implanted material in all types of infection,
whatever the clinical presentation.
19
In our study, we used conservative treatment and we had
four out of six recurrences. Mortality was one in six (16.7%)
patients. This highlights the importance of complete removal and
re-implantation of a new device or a sterilised, used pacemaker,
especially in our circumstances.
Conclusion
Infections secondary to pacemaker implantation are rare but
serious. The risk factors found were diabetes, dermatoses, longer
duration of in-hospital pre-operative stay, use of a temporary
pacemaker, the number of patients in the ward, postoperative
haematoma and re-operation. The management of infection is
difficult and can lead to removal of the implanted device. Hence
the importance of prevention, especially in our country where
pacemakers are still very expensive.
References
1.
Klug D, Balde M, Pavin D,
et al
.
Risk factors related to infections of
implanted pacemakers and cardioverter-defibrillators: results of a large
prospective study.
Circulation
2007;
116
: 1349–1355.
2.
Selton-Suty C, Doco-Lecompte T, Freysz L,
et al.
L’endocardite sur
matériel de stimulation intracardiaque.
Ann Cardiol Angeiol
2008;
57
:
81–87.
3.
Camus C, Donal E, Bodi S,
et al.
Infections liées aux pacemakers et
défibrillateurs implantables.
Med Mal Infect
2010;
40
: 429–439.
4.
Catanchin A, Murdock CJ, Athan E.
Pacemaker infections: a 10-year
experience.
Heart Lung Circ
2007;
16
: 434–439.
5.
Uslan DZ, Sohail MR, St Sauver JL,
et al
.
Permanent pacemaker and
implantable cardioverter defibrillator infection: a population-based
study.
Arch Intern Med
2007;
167
: 669–675.
6.
Kearney RA, Eisen HJ, Wolf JE. Nonvalvular infections of the cardio-
vascular system.
Ann Intern Med
1994;
121
: 219–230.
7.
Villamil Cajoto I, Rodriguez Framil M, van den Eynde Collado A,
et al
.
Permanent transvenous pacemaker infections: an analysis of 59 cases.
Eur J Intern Med
2007;
18
: 484–488.
8.
Sohail MR, Uslan DZ, Khan AH,
et al
.
Risk factor analysis of perma-
nent pacemaker infection.
Clin Infect Dis
2007;
45
: 166–173.
9.
Marschall J, Hopkins-Broyles D, Jones M,
et al
.
Case-control study of
surgical site infections associated with pacemakers and implantable
cardioverter-defibrillators
.
Infect Control Hosp Epidemiol
2007;
28
:
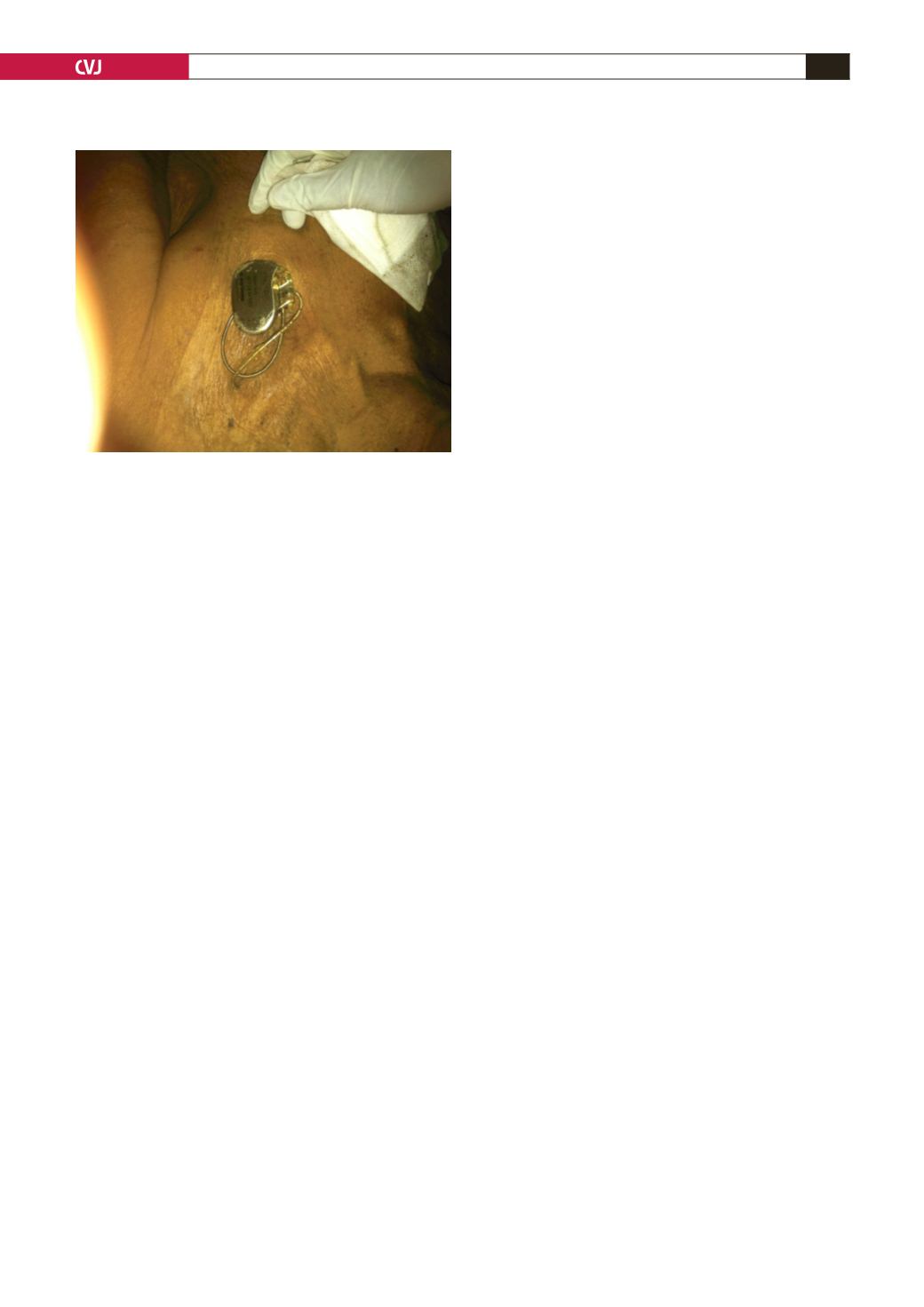
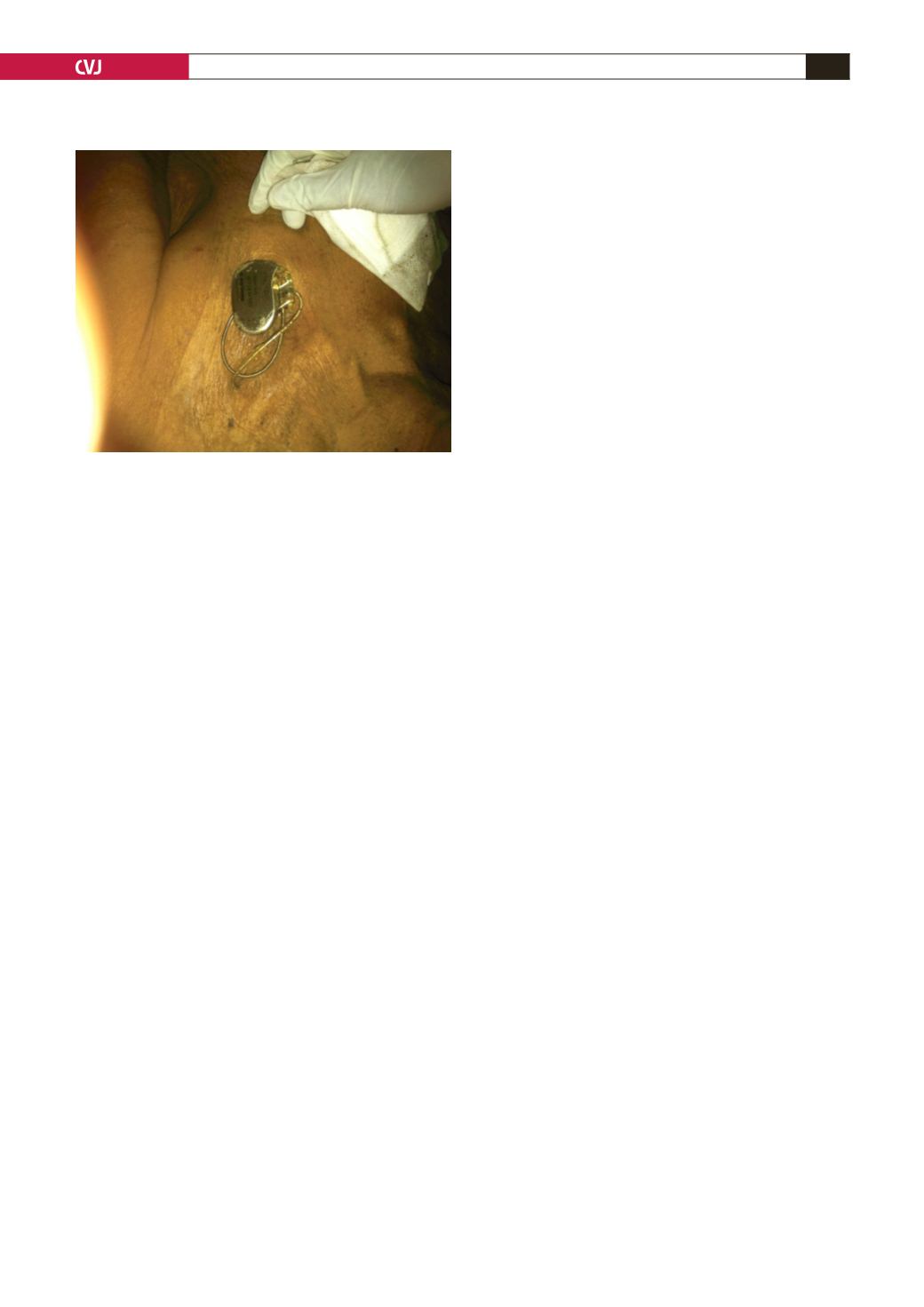
Fig. 1. Externalisation of the pacemaker pouch.