CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 4, May 2012
AFRICA
225
Furthermore, hyperglycaemia is also known to activate
protein kinase C (PKC), which decreases eNOS activity, leading
to reduced NO and increased ET-1 production.
24
In the setting
of ED, ET
B
receptor-mediated vasodilatory effects of ET-1 are
blunted (refer to Table 1) and therefore the vasoconstrictory state
predominates.
26
PKC also enhances the expression of adhesion
molecules such as ICAM, VCAM and E-selectin,
24
which is
associated with endothelial cell activation.
ED has been reported to occur early in insulin resistance.
22
Often insulin resistance is associated with central adiposity
and hence the metabolic syndrome, i.e. hypertriglyceridaemia,
low high-density lipoprotein (HDL) levels, high low-density
lipoprotein (LDL) levels and hypertension, all of which could
potentially favour the development of ED and eventually
atherogenesis.
22
Hyperlipidaemia
Hyperlipidaemia constitutes increased circulating lipids including
cholesterol and triglycerides, a state which can predispose to ED.
Possible mechanisms underlying hyperlipidaemia-induced ED
include: (1) upregulation of NADPH oxidase, increased O
2
–
production and oxidative stress, (2) increased plasma levels of
asymmetric dimethylarginine (ADMA),
25
and (3) oxidation of
LDL.
27
ADMA is an endogenous inhibitor of eNOS and competes
with L-arginine for the same binding site on eNOS, thus resulting
in eNOS uncoupling, increased O
2
–
production and hence
decreased NO production. Plasma concentrations of ADMA
have been reported to be increased in hypercholesterolaemia,
28,29
and this compound is considered to be both a marker and risk
factor of ED.
28
In addition to scavenging NO, excess O
2
–
modifies LDL
cholesterol to form oxidised LDL (ox-LDL), which plays a
major role in the development of endothelial activation and
atherogenesis.
30
Ox-LDL has been reported to promote ET-1
production,
31
expression of adhesion molecules and chemo-
attractants, as well as VSMC migration and proliferation.
27
Furthermore, ox-LDL can be engulfed by macrophages forming
foam cells which adhere to the vessel wall and contribute to the
initiation of an atherosclerotic plaque.
27
Both LDL and ox-LDL have been shown to increase the
activity of S-adenosylmethionine-dependent methyltransferases,
which lead to increased ADMA synthesis. Therefore, LDL and
ox-LDL may be accountable for the increased plasma levels of
ADMA in hypercholesterolaemia.
32
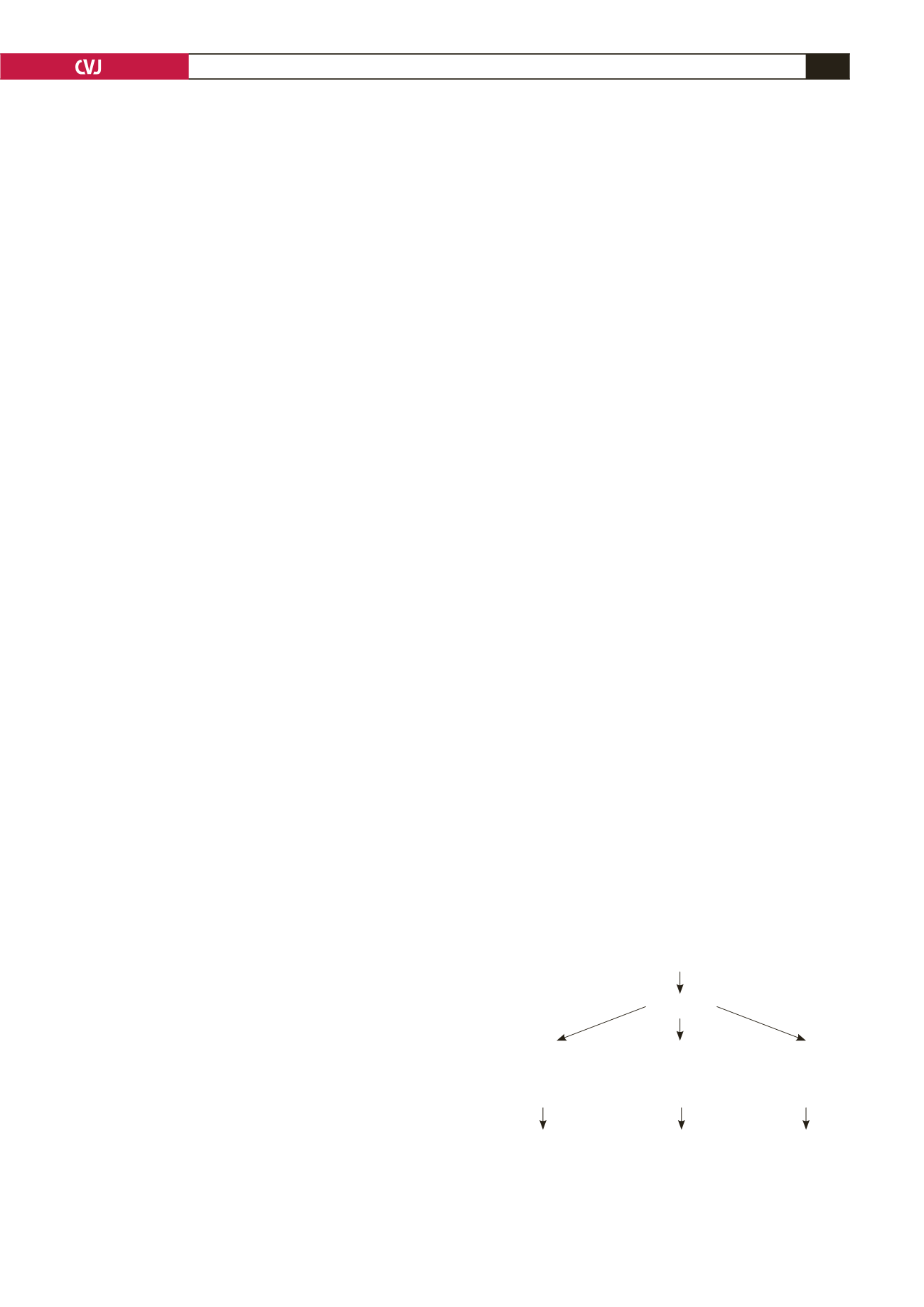
LDL or ox-LDL can also
upregulate caveolin-1 synthesis and thus inhibit eNOS activity
33,34
(Fig. 4).
Hypertension
ED is a prominent underlying feature of hypertension,
35
and
patients with hypertension have been shown to demonstrate
blunted forearm blood flow in response to vasodilatory stimuli
such as acetylcholine and bradykinin,
36
which is indicative
of ED. Increased production of ROS and endothelial-derived
contracting factors (EDCFs) such as ET-1, angiotensin II, PGH
2
and TXA
2
, and decreased NO bioavailability are all observed in
patients with hypertension.
26,36
Shear stress is known to be one of the most important
mechanisms of inducing NO-mediated vasodilation in both
the micro- and macrovasculature. However, this response is
reduced or absent in hypertensive patients.
37
In addition to this,
Iaccarino
et al
.
38
observed decreased protein kinase B (PKB)/
Akt-dependent activation of eNOS in a model of spontaneously
hypertensive rats (SHR).
In a recent study, the role of oxidative stress and ED in the
development of hypertension in spontaneously hypertensive rates
was investigated.
35
The results showed that early treatment with
the antioxidant reservatrol was associated with reduced oxidative
stress markers, improved endothelium-dependent vasodilatation
and an attenuation in the development of hypertension in these
animals.
Smoking
Tobacco smokers exhibit decreased NO bioavailability, increased
levels of ox-LDL, and impaired flow-mediated vasodilation,
phenomena which are all highly suggestive of ED.
39
Passive
smoking has recently also been implicated in impairment of
endothelial function.
39,40
It appears that the harmful effects of
smoking on endothelial cells are dose dependent and reversible
upon smoking cessation.
39
As with other cardiovascular disease
risk factors, oxidative stress appears to be the major mechanistic
link between smoking and ED.
39,41
Cigarette smoke is rich in free radicals and directly delivers
free radicals to the body. Besides being the supplier of free
radicals, cigarette smoke facilitates endogenous release of ROS
via activation of inflammatory cells.
41,42
Furthermore, smoking
has been reported to decrease the levels of HDL cholesterol,
which is known to have anti-endothelial dysfunction and anti-
atherosclerotic properties.
43
Aging
Increasing age has been recognised as one of the factors that
predisposes to ED.
43,44
With aging, the ability of the endothelium
to produce NO is reduced.
45
Furthermore, some studies have
reported reduced expression and activity of eNOS as well as
decreased expression of a major downstream target molecule of
NO, soluble guanylyl cyclase (sGC) in VSMCs, and its activity in
older animals.
45
In addition to the decreased NO production, other
endothelial-derived relaxing factors (EDRFs) (prostacyclin and
EDHF) are also reduced, while endothelial-derived contracting
factors (EDCFs) such as ET-1 and COX-derived prostanoids,
and ROS production are increased.
44,45
Plasma levels of ADMA
Fig. 4. Pathophysiological effects and the interplay
between increased plasma cholesterol and O
2
–
levels, and
endothelial cell responses.
↑
cholesterol + O
2
–
Endothelial
activation
Endothelial
dysfunction
Atherosderotic
plaque
ox-LDL
Endothelial cells:
↑
endothelin–1
↑
adhesion molecules
↑
ADMA,
↑
caveolin–1:
eNOS coupling
↓
eNOS activation
↓
NO bioavailability
+
Macrophages
Foam cells