CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 4, May 2012
220
AFRICA
of postpartum haemorrhage (Table 6) following the switching
of anticoagulants. These cases occurred at C/S, highlighting
the need for intense monitoring of coagulation indices at
this time. McLintock
et al.
also reported high rates of ante-
and postpartum haemorrhagic complications using LMWH
throughout pregnancy.
11
A number of studies report that UH and LMWH therapy is
safe for the foetus.
21,23
Unfractionated heparin does not cross the
placenta and does not have the potential to cause foetal bleeding
or teratogenecity. Heparin is generally considered safer than
warfarin during pregnancy in terms of embryopathy, however
the efficacy of heparin in the prevention of thrombo-embolic
complications during pregnancy is contentious. Several reports
indicate that its use is associated with high incidence of thrombo-
embolic complications, including fatal valve thrombosis in
high-risk pregnant women managed with subcutaneous UH and
LMWH therapy.
18,19,22,23
Chan
et al.
reviewed pregnancy outcomes in women with
MPHV and reported thrombo-embolic complications in 3.9% of
pregnancies using warfarin only; 9.2% in women who received
UH in the first trimester followed by warfarin, and 33% in
pregnancies treated with UH heparin throughout pregnancy.
14
Oran
et al.
reviewed pregnant women with MPHV managed
with LMWH and reported complications related to valve
thrombosis in 10/81 pregnancies.
28
Similarly, another review
reported thrombotic events in 22% of pregnant women (
n
=
76)
managed with LMWH.
29
More recently, data are emerging that dose-adjusted LMWH
(enoxaparin) may be administered safely in pregnancy when
there is a dosage adjustment throughout pregnancy to maintain
an anti-Xa of 1.0–1.2 U/ml.
30
There were no thrombo-embolic
events in this study of 15 women with MHVP. These reports
follow a randomised study in South Africa, comparing UH with
enoxaparin, which was stopped prematurely because of two
deaths from thrombo-embolism in the enoxaparin group. Anti-
Xa levels were measured but no dose adjustment was done.
31
There is evidence that increasing doses of heparin are required
with increasing gestational age because of the increased blood
volume and greater renal clearance as pregnancy progresses.
30
There was one maternal death in our study. Earlier studies
originating from under-resourced countries have reported two
maternal deaths in 312 patients studied,
4
one in 229 patients,
32
and 10 in 480 patients studied.
33
There was a high rate of maternal complications in our study.
Four (7%) patients on warfarin
≥
5 mg daily developed valve
thrombosis in the mitral position. The mitral position is prone to
thrombosis and our audit confirms similar findings from other
studies.
31,34
Throbo-embolic events and embryopathy are not the only
risks that are associated with pregnancies in women with
MHVP. Atrial fibrillation, infective endocarditis and C/S wound
haematomas were relatively common complications observed in
our study.
Conclusions
This study confirms that the use of warfarin throughout pregnancy
carries a significant risk of embryopathy. This risk may be
greater with doses of
>
5 mg but no definite conclusions can be
drawn. In addition, the use of warfarin in the second trimester of
pregnancy is associated with significant foetal losses, probably
due to poor monitoring and control of warfarin dosages. The
switching of warfarin to heparin at the time of delivery may be
associated with maternal complications.
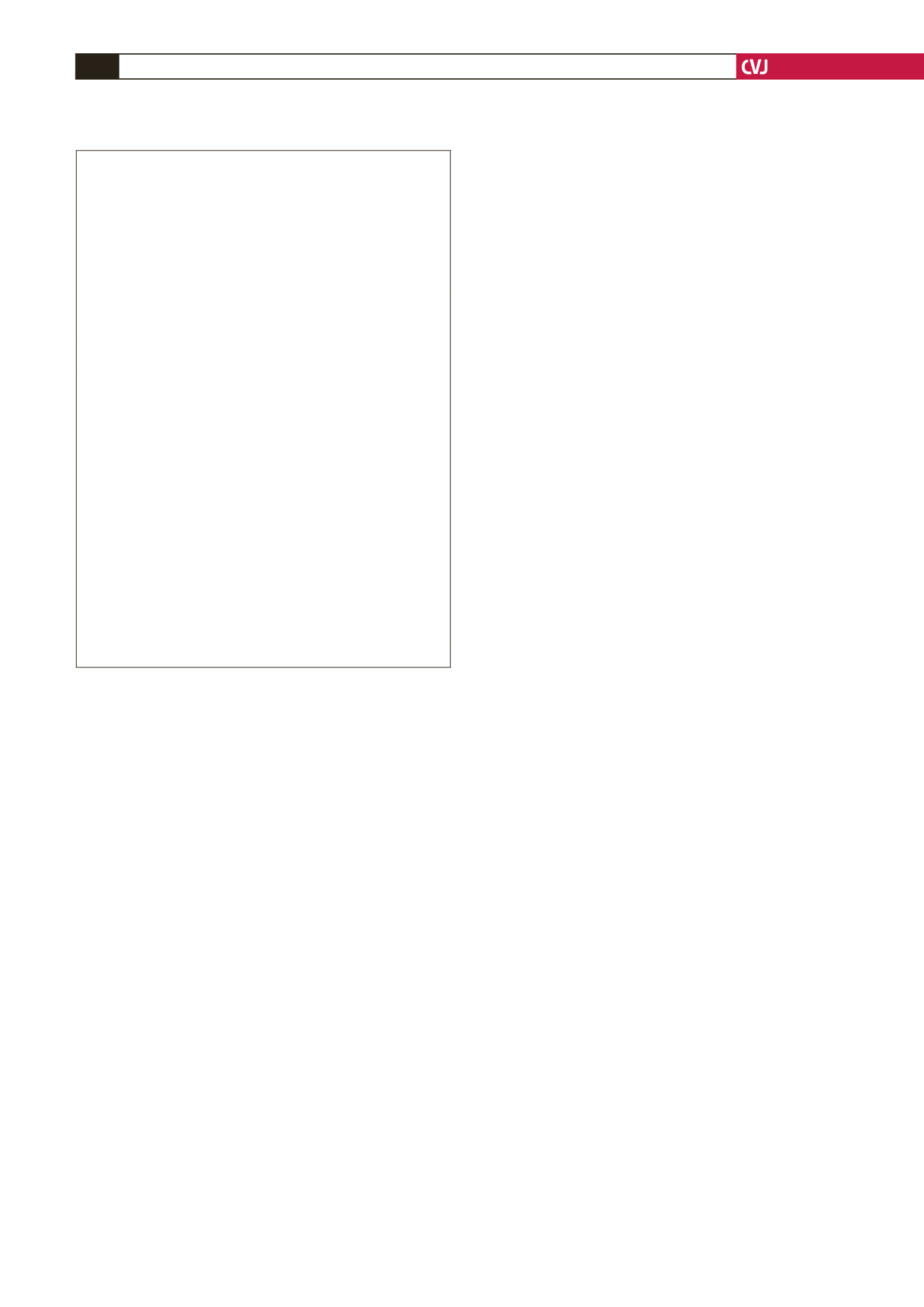
Recommendations for management of anticoagulation in
pregnant women with MHVP are found in guidelines produced
by the American College of Cardiology/American Heart
Association.
35
These guidelines are based on the opinions of
experts. An anticoagulation regimen reported by Pieper
et al.
has been modified and shown in Table 7;
8
and takes into account,
the key points of the American guidelines. Large randomised
trials of dose-adjusted LMWH are necessary before firm
recommendations on an acceptable prophylaxis anticoagulation
regimen for prevention of thrombosis of MHVP can be made.
References
1.
Nassar AH, Hobeika EM, Abol Wssarmad HM,
et al.
Pregnancy
outcome in women with prosthetic heart valves.
Am J Obstet Gynecol
2004;
191
: 1009–1013.
2.
Sbarouni E, Oakley CM. Outcome of pregnancy in women with valve
prostheses.
Br Heart J
1994;
71
:
196–201.
3.
Nqayana T, Moodley J, Naidoo DP. Cardiac disease in pregnancy.
Cardiovasc J South Afr
2008;
19(3
):145–151.
4.
Malhotra M, Sharma JB, Tripathii R, Arora P, Arora R. Maternal and
fetal outcome in vavular heart disease.
Int J Gynaecol Obstet
2004:
84
: 11–16.
5.
Saving Mothers: A report of the National Committee on Confidential
Enquiries into Maternal Deaths: 2005–2007. Pretoria: Department of
Health, 2008.
6.
Shannon MS, Edwards MB, Long F,
et al.
Anticoagulant manage-
ment of pregnancy following heart valve replacement in the United
Kingdom, 1986-2002.
J Heart Valve Dis
2008;
17
(5): 526–532.
TABLE 7.ANTICOAGULATION REGIMEN IN PREGNANT
WOMENWITH MECHANICAL PROSTHETICVALVES
Pre-pregnancy
• Discuss anticoagulation regimen with patient
• Continue warfarin until pregnancy is achieved
• When menstruation is delayed, perform pregnancy test every few days
until positive or until menstruation (in order to detect pregnancy at an
early stage)
• Give patient and health professional responsible for anticoagulation
written instructions about anticoagulation regimen during pregnancy
Sixth to 12th week of pregnancy
• If warfarin daily dose is
<
5 mg, consider continuation of warfarin
throughout pregnancy
• Alternatively, substitute warfarin with subcutaneous LMWH twice
daily
• Adjust LMWH dose to achieve peak anti-Xa levels of 0.7–1.2 U/ml
four hours post dose
• If trough levels are sub-therapeutic with therapeutic peak levels, dose
three times daily
• Check anti-Xa levels twice a month
13th to 35th week of pregnancy
• Resume warfarin
• Or use LMWH adjusted dose
36th week of pregnancy
• Substitute warfarin with subcutaneous LMWH twice daily
• Adjust LMWH dose to achieve peak anti-Xa levels of 0.7–1.2 U/ml
four hours post dose
• If trough levels are sub-therapeutic with therapeutic peak levels, dose
three times daily
• Check anti-Xa levels weekly