CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 3, May/June 2014
AFRICA
111
blood was collected in tripotassium EDTA tubes. We analysed
the blood samples using an automatic blood counter within one
hour of drawing the blood.
The patients underwent a two-day stress/rest single-photon-
emission tomography and gated GSPECT study using adenosine
with a standard weight-based infusion protocol (140 μg/kg/min).
The six-minute adenosine infusion was begun and 740 MBq (20
mCi) of MIBI was injected after three minutes. After a 45-minute
delay, a stress set of images was acquired.
At rest, before receiving technetium-99m methoxy isobutyl
isonitrile (
99m
Tc-MIBI), the patients were given one to two tablets
of sublingual nitroglycerin (0.4 mg), five minutes apart and they
were injected with 740 MBq (20 mCi) of MIBI. A GSPECT
study was performed 45 minutes later.
GSPECT data were acquired in the supine position with the
double-head SPECT-
γ
camera equipped with a high-resolution
low-energy collimator. The obtained data were projected as
myocardial tomographic slices in short-axis, vertical long-axis
and horizontal long-axis views. Electrocardiogram gating was
applied to the cardiac cycle with eight frames per cardiac cycle.
The myocardium was divided into 17 segments following the
American Society of Nuclear Cardiology/American College of
Cardiology/American Heart Association guidelines.
8
GSPECT dates were processed and analysed using
4D-MSPECT software, which determines the extent and severity
of left ventricular perfusion defect size and the extent of
reversible (ischaemia) or fixed (scar) perfusion defects.
9
The
programme assigned a score of 0 to 4 to each segment based on
activity level: 0
=
normal, 1
=
equivocal, 2
=
moderate, 3
=
severe
reduction of radioisotope uptake, and 4
=
absence of detectable
tracer uptake. Abnormal perfusion, motion and thickening were
defined as a score of
≥
2.
The summed stress score (SSS), summed rest score (SRS),
and summed difference score (SDS) were calculated based on
the conventional 17-segment model. The summed difference
score (SDS), indicating the extent of reversible perfusion defects,
was obtained by calculating the differences between the SSS and
SRS.
Statistical analysis
Statistical analyses were performed using SPSS 18.0 software.
Parametric values are given as mean
±
standard deviation and
non-parametric values as a percentage. To compare parametric
continuous variables, the Student’s
t
-test was used; to compare
non-parametric continuous variables, the Mann–Whitney
U
-test was used. Categorical data were compared by chi-square
distribution. Stepwise multivariate logistic regression models
were created to determine independent variables for myocardial
perfusion defect. For multivariate regression, variables with a
p
-value
<
0.1 in univariate analysis were selected. Two-tailed
p
-values
<
0.05were considered to indicate statistical significance.
Results
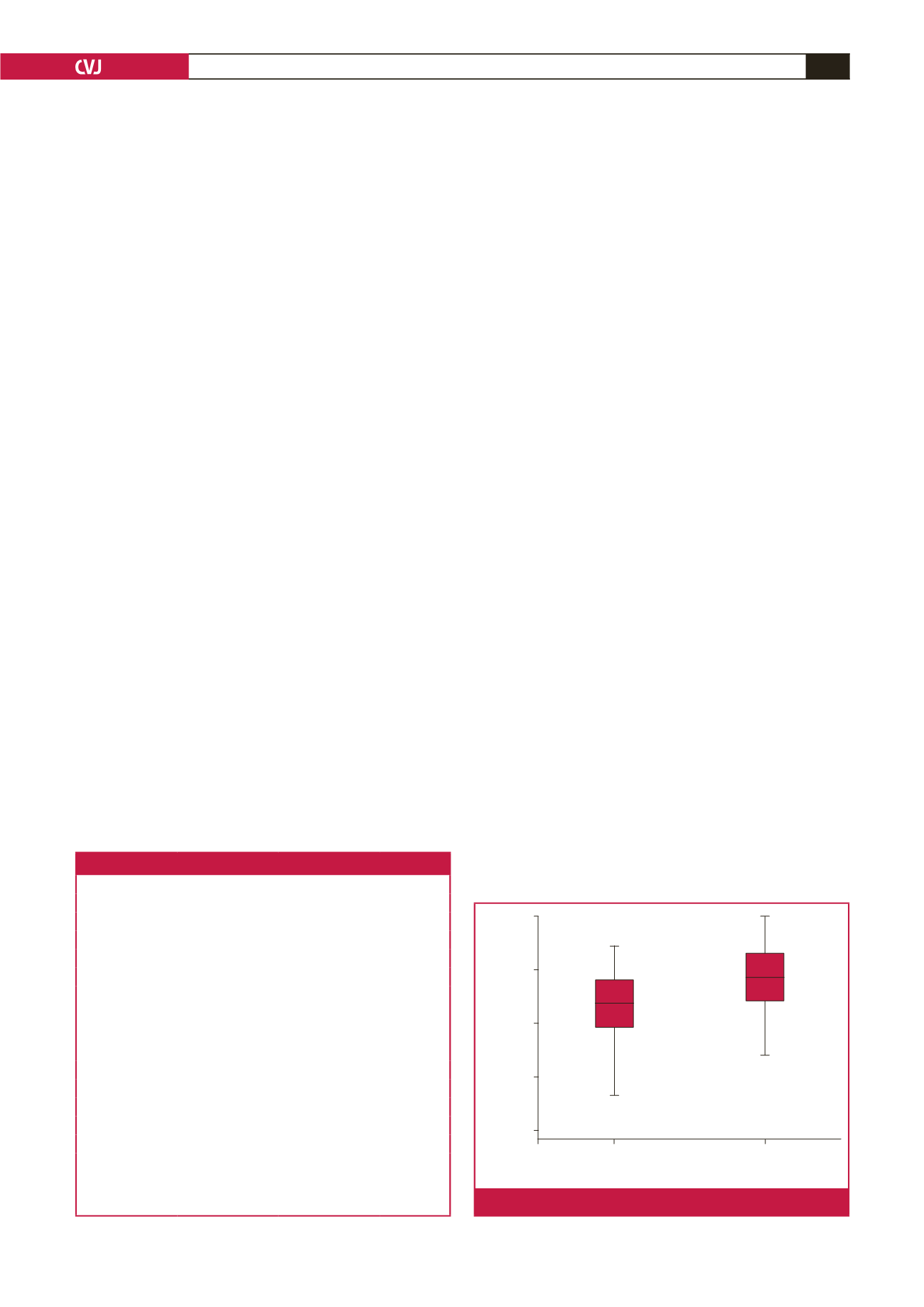
Baseline characteristic of the patients are given in Table 1. Levels
of glucose, triglycerides (TG), total cholesterol (TC), low-density
lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL)
cholesterol, haemoglobin (Hb) and glycosylated haemoglobin
(HbA
1c
), and body mass index (BMI) in the two groups were not
statistically significantly different. The MPV level was higher in
group 1 than in group 2 patients (8.76
±
0.78 and 8.25
±
0.78 fl,
respectively,
p
=
0.003). Levels of MPV in the two groups are
shown in Fig. 1.
Univariate analysis showed that MPV, and HbA
1c
and glucose
levels were significantly involved in myocardial perfusion
defects. Multivariate logistic regression analyses showed that
MPV was the only variable independently associated with
myocardial perfusion defect (OR: 2.401, 95% CI: 1.298–4.440,
p
=
0.013) (Table 2).
Discussion
This study showed that there was a relationship between
myocardial perfusion defect and MPV. MPV was higher in the
group with myocardial perfusion defects, compared to the one
without myocardial perfusion defects. Patients with diabetes
develop vascular complications, including macrovascular
complications [coronary artery disease (CAD), peripheral
vascular disease and stroke] and microvascular complications
[diabetic nephropathy (DN), diabetic retinopathy (DR) and
Table 1. Baseline characteristic of the patients.
Group 1
Group 2
p
-value
Age (years)
60.02
±
9.28
60.81
±
8.02
0.660
Women (%)
72.7
68.2
0.408
HT (%)
72.7
86.4
0.093
HL (%)
47.7
56.8
0.281
Aspirin (%)
34.1
29.5
0.410
BMI (kg/m
2
)
31.41
±
6.23
30.41
±
5.7
0.446
Glucose (mg/dl)
131.79
±
40.553 151.16
±
54.213
0.070
TG (mg/dl)
192.36
±
116.48 171.71
±
87.321
0.600
TC (mg/dl)
190.04
±
42.25 178.83
±
46.73
0.258
HDL-C (mg/dl)
40.58
±
5.911
38.68
±
6.08
0.167
LDL-C (mg/dl)
118.77
±
28.75 108.28
±
33.82
0.133
Hb (g/dl)
13.16
±
1.40
13.42
±
1.46
0.399
MPV (fl)
8.76
±
0.76
8.25
±
0.78
0.003
HbA
1c
(%)
8.67
±
0.68
8.35
±
0.86
0.094
HT: hypertension; HL: hyperlipidaemia TG: triglycerides; TC: total
cholesterol; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-
density lipoprotein cholesterol; Hb: haemoglobin; MPV: mean platelet
volume; HbA
1c
: glycosylated haemoglobin.
10.00
9.00
8.00
7.00
6.00
MPD (–)
MPD (+)
Groups
MPV
Fig. 1.
MPV levels in the two groups.