CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 3, May/June 2014
112
AFRICA
peripheral neuropathy].
10
Continuous hyperglycaemia may cause
endothelial dysfunction and vascular lesions, resulting in diabetic
vascular complications.
11,12
Type 2 diabetes is a substantial risk factor in atherosclerotic
cardiovascular disease.
13,14
Cardiovascular disease (CVD) is the
leading cause of death in patients with type 2DM.
15
Asymptomatic
CAD is common in patients with DM and is a strong predictor
of future poor outcome of coronary vascular events, as well as
early death.
16,17
DM is associated with generalised endothelial
dysfunction and small-vessel abnormalities.
18,19
Perfusion defects are substantial predictors of coronary
events in patients with known or suspected coronary heart
disease (CHD).
20
It is proposed that concomitant abnormalities
of perfusion imaging scans in patients with diabetes with normal
coronary angiograms may be caused by micro-angiopathy or
endothelial dysfunction. Accordingly, it reflects an increased
likelihood of future coronary events.
21
The majority of studies on ischaemia have used SPECT MPI.
An analysis of the diagnostic accuracy of pharmacologically
induced stress MPI reported a mean sensitivity and specificity
of 88 and 77%, respectively.
22
Platelet volume is a marker of platelet activation and function,
and is measured usingMPV.
5
Platelets that have dense granules are
more active biochemically, functionally and metabolically. Large
platelets secrete high levels of prothrombogenic thromboxaneA2,
serotonin, beta-thromboglobulin and procoagulant membrane
proteins such as P-selectin and glycoprotein IIIa.
5,23
Platelets
secrete a large number of substances that are crucial mediators
of coagulation, inflammation, thrombosis and atherosclerosis.
24,25
It is also well known that large platelets are a risk factor
for developing coronary thrombosis, leading to myocardial
infarction.
19,23,26,27
Measurement of platelet activation and/or aggregation may
provide prognostic information in patients at risk for or following
a cardiovascular event.
28,29
Reports have revealed that there is a
close relationship between MPV and cardiovascular risk factors,
including impaired fasting glucose levels, diabetes mellitus,
hypertension, hypercholesterolaemia, obesity and the metabolic
syndrome.
30-32
Increased platelet activity is reported to play a
role in the development of vascular complications in diabetic
patients.
18
MPV was increased in patients with SCF complex and cardiac
syndrome X, both being related to microvascular defects and
endothelial dysfunction.
33,34
In the present study, we showed that
MPV was associated with myocardial perfusion defect, using
MPI in diabetic patients.
In our study, MPV was increased in the myocardial perfusion
defect group compared to those without myocardial perfusion
defects. DM not only involves the main coronary artery but also
the microvascular circulation, leading to myocardial perfusion
defects. Perfusion defects are significant predictors of coronary
events in patients with known or suspected CHD.
20
The main limitation of our study was the small sample size,
which could result in low statistical power for equivalency
testing, leading to false-negative results. Second, because of the
retrospective nature of data collection, the angiographic results
of the patients were not evaluated. MPI may reflect myocardial
perfusion defects but it was not able to show the anatomical
status of the coronary artery. We cannot extend our results to the
general population due to our broad exclusion criteria.
Conclusion
MPV levels were higher in the diabetic patients with myocardial
perfusion defects than in those without myocardial perfusion
defects. In diabetic patients, increased MPV may be an
independent marker of myocardial perfusion defects, which are
associated with adverse coronary events.
References
1.
Whiteley L, Padmanabhan S, Hole D, Isles C. Should diabetes be
considered a coronary heart disease risk equivalent? results from 25
years of follow-up in the Renfrew and Paisley survey.
Diabetes Care
2005;
28
: 1588–1593.
2.
Kannel WB, McGee DL. Diabetes and cardiovascular disease. The
Framingham study.
J Am Med Assoc
1979;
241
: 2035–2038.
3.
Nathan DM, Meigs J, Singer DE. The epidemiology of cardiovascular
disease in type 2 diabetes mellitus: how sweet it is ... or is it?
Lancet
1997;
350
(Suppl 1): SI4–9.
4.
Misko J. Evaluation of myocardial perfusion and viability in coronary
artery disease in view of the new revascularization guidelines.
Nuclear
Med Rev Central Eastern Eur
2012;
15
: 46–51.
5.
Martin JF, Shaw T, Heggie J, Penington DG. Measurement of the densi-
ty of human platelets and its relationship to volume.
Br J Haematol
1983;
54
: 337–352.
6.
Erhart S, Beer JH, Reinhart WH. Influence of aspirin on platelet count
and volume in humans.
Acta Haematol
1999;
101
: 140–144.
7.
Zuberi BF, Akhtar N, Afsar S. Comparison of mean platelet volume
in patients with diabetes mellitus, impaired fasting glucose and non-
diabetic subjects. S
ingapore Med J
2008;
49
: 114–116.
8.
Cerqueira MD, Weissman NJ, Dilsizian V,
et al
. Standardized myocar-
dial segmentation and nomenclature for tomographic imaging of
the heart. A statement for healthcare professionals from the Cardiac
Imaging Committee of the Council on Clinical Cardiology of the
American Heart Association.
Circulation
2002;
105
: 539–542.
9.
Ficaro EP, Lee BC, Kritzman JN, Corbett JR. Corridor4DM: the
Michigan method for quantitative nuclear cardiology.
J Nucl Cardiol
2007;
14
: 455–465.
10. Murea M, Ma L, Freedman BI. Genetic and environmental factors
associated with type 2 diabetes and diabetic vascular complications.
Rev Diabet Studies
2012;
9
: 6–22.
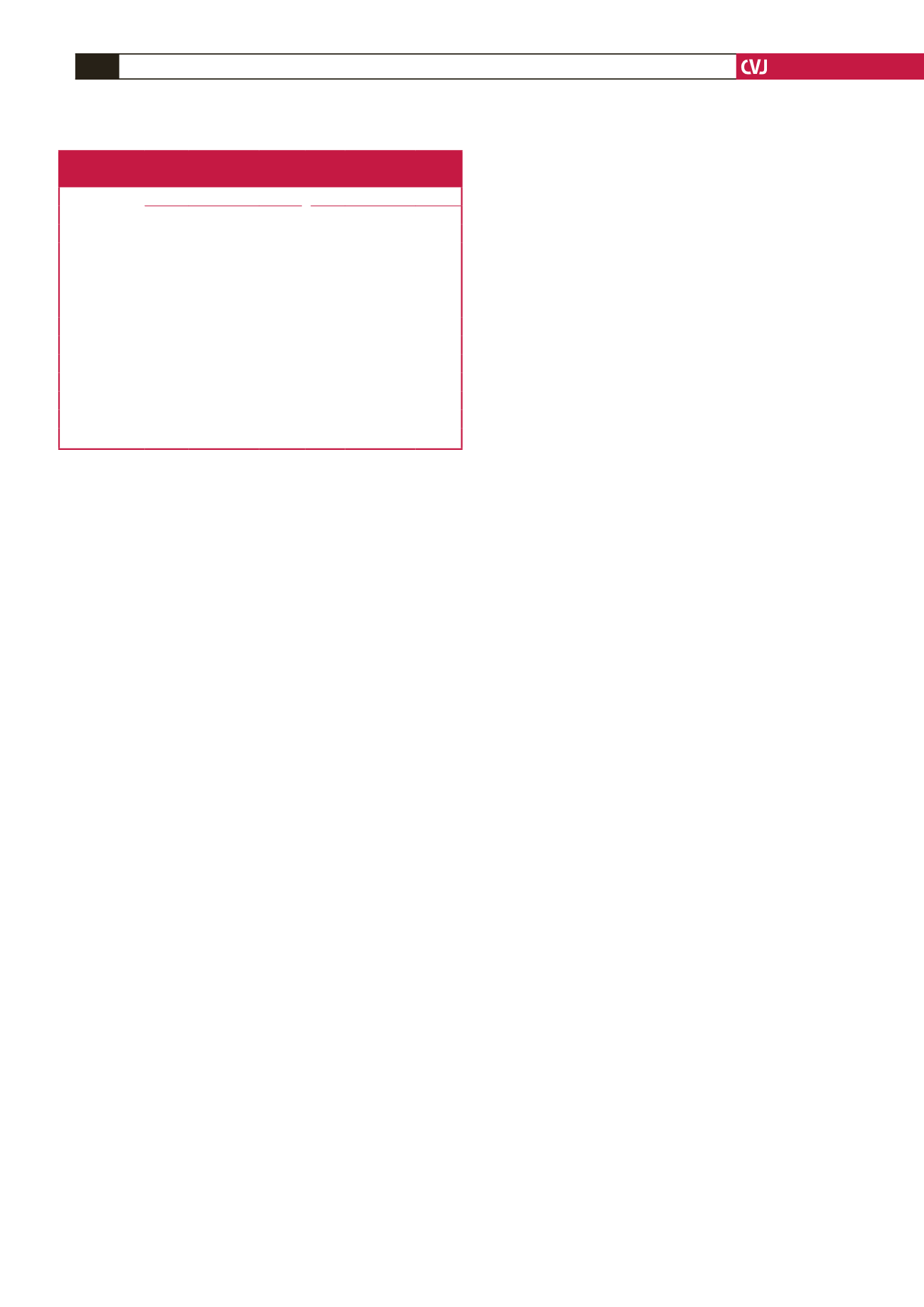
Table 2. Univariate and multivariate regression analyses of
independent variables for MPD.
Univariate
Multivariate
Variables
OR 95% CI
p
-value OR
95% CI
p
-value
MPV (fl)
2.401 1.298–4.440 0.005 2.484 1.215–5.081 0.013
Glucose (mg/dl) 1.009 0.999–1.029 0.072 1.008 0.997–1.019 0.178
HbA
1c
(%)
1.800 0.993–3.474 0.08 1.984 0.980–4.018 0.064
Age (years)
1.011 0.963–1.061 0.664
Gender
1.244 0.497–3.16 0.641
HT (mg/dl)
2.375 0.801–7.043 0.119
BMI (km/m
2
)
0.991 0.92–1.067 0.820
TC (mg/dl)
0.994 0.984–1.004 0.256
TG (mg/dl)
0.998 0.994–1.002 0.360
HDL-C (mg/dl) 0.948 0.878–1.023 0.167
LDL (mg/dl)
0.989 0.975–1.003 0.134
Hb (%)
1.138 0.845–1.534 0.395