CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 6, November/December 2014
AFRICA
e7
2–3/6 holosystolic murmur at the apex. Respiratory system
examination revealed rough breathing sounds, but there were no
rales or rhonchi.
Chest X-ray showed a mildly increased cardiothoracic index.
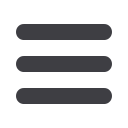
The electrocardiogram (ECG) showed wide QRS complex
tachycardia (Fig. 1). The QRS duration was 150 ms. In the
emergency department, adenosine (12 mg iv) was given to the
patient to eliminate the supraventricular tachycardia but there
was no response in rhythm or rate.
Her basic laboratory findings were glucose: 149 mg/dl, urea:
103 mg/dl, creatinine: 1.02 mg/dl, potassium: 4.03 mg/dl, uric
acid: 11.1 mg/dl, AST: 1601 U/l, ALT: 1679 U/l, INR: 2.18.
When the laboratory findings and imaging tests were evaluated
together with the findings of the physical examination, forefront,
ischaemic hepatitis and prerenal azotaemia showing end-organ
damage were considered.
Because the haemodynamic parameters were unstable and
critical end-organ damage had developed, emergency electrical
cardioversion (100 J) was performed. After cardioversion,
pacemaker rhythm (60 beats/min) was maintained (Fig. 2) and
the blood pressure was 125/75 mmHg.
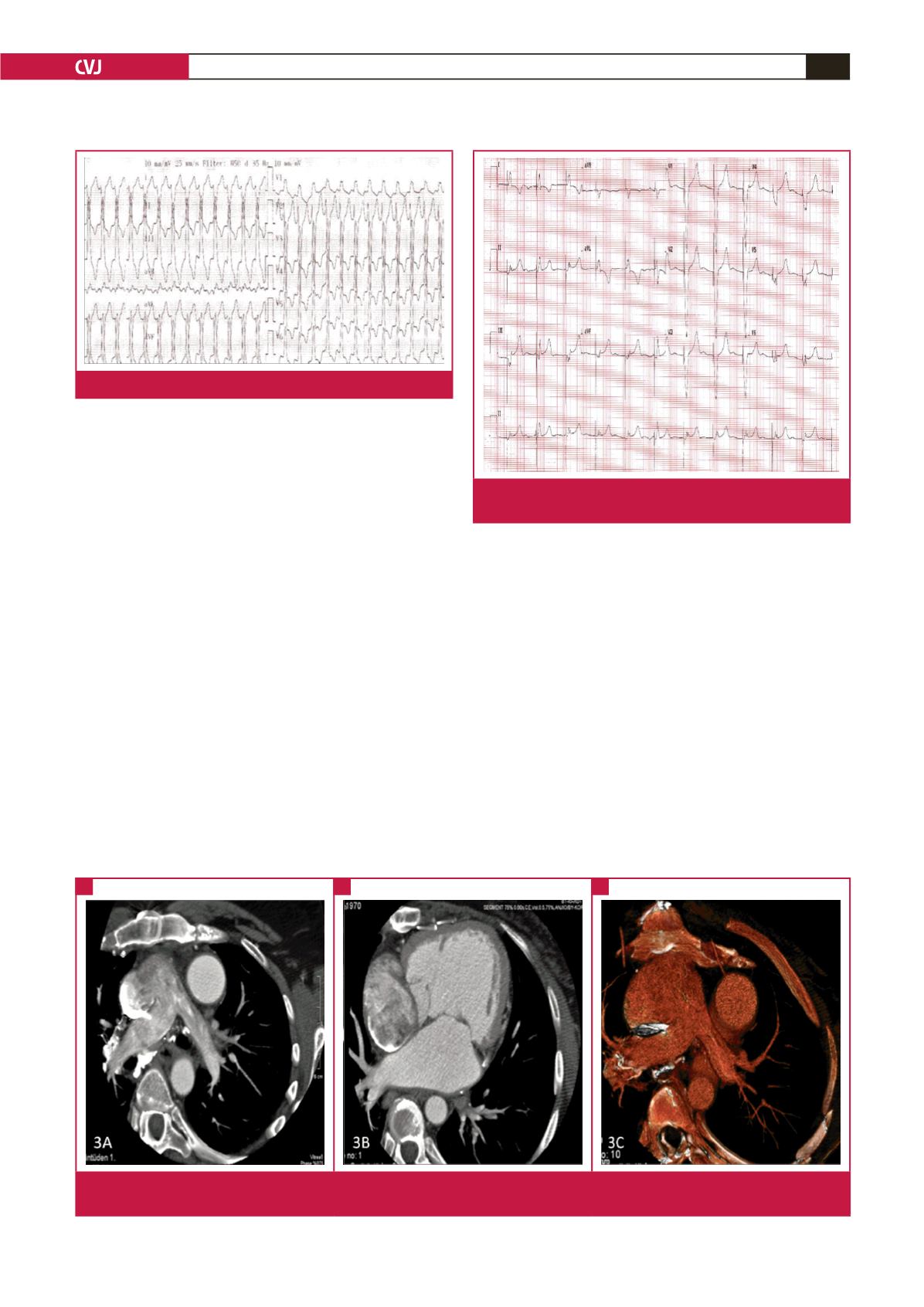
Transthoracic echocardiogram (TTE) revealed a rudimentary
interventricular septum with hypoplastic right ventricle and
functional single (left) ventricle, a conduit between the right
atrium and pulmonary artery, left atrial dilatation, severe
mitral regurgitation (eccentric) and systolic dysfunction with an
ejection fraction (EF) of 30% (Fig. 3). Considering structural
heart disease with decreased LVEF (< 30%) and spontaneous
sustained episodes of ventricular tachycardia (VT), the patient
had class I (evidence level B) indication for ICD implantation,
according to the recent guidelines.
4
The cardiac anatomy and venous system was scanned with
cardiac computerised tomography (CT) to evaluate for lead
placement. On CT, the arcus aorta was located on the left, the
left anterior descending artery and right coronary artery were
emerging from the same cusp adjacently, and the circumflex
artery was emerging from another cusp. The right ventricle was
significantly hypoplastic and associated with the left ventricle,
there was no main pulmonary artery, and the pulmonary
arteries were connected to the right atrium (Fig. 4). Since the
conventional transvenous access to the markedly hypoplastic
right ventricle was impossible, an epicardial ICD implantation
was planned.
Fig. 1.
ECG showing wide QRS complex tachycardia.
Fig. 2.
Pacemaker rhythm (60 bpm) was observed on ECG
after cardioversion.
Fig. 3.
A, B, CT scan showing systemic venous blood entering the pulmonary circulation through a cavopulmonary conduit. C, a
hypoplastic right ventricle associated with the left ventricle was seen on CT scan.
A
B
C



















