CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 6, November/December 2014
AFRICA
e9
for implantation were VT and ventricular dysfunction in two,
VT and syncope in one, and resuscitated sudden cardiac death
in one patient. All underwent a midline sternotomy with surgical
placement of a subcutaneous ICD coil into the pericardial sac.
In addition to the ICD lead, a second epi-myocardial bipolar
lead was placed on the ventricle for sensing and pacing in all
patients. All patients had a defibrillation threshold of < 20 J.
There were no complications at a mean follow-up period
of 22 months despite it being thought that the intrapericardial
defibrillation coil could lead to pericarditis, adhesions,
infection and pericardial thickening. We have not observed any
complications related to epicardial ICD coils in our patients to
date. Although defibrillation coil lead dislodgment from the
pericardium is a concern, stabilising the tip and body of the
coil in a halo shape and securing the lead to the surrounding
tissue, as used in our technique, should stabilise the lead in the
pericardium.
In another case series, eight patients were identified who had
undergone ICD placement or revision requiring non-traditional
alternative surgical lead placement.
21
One had undergone the
Fontan procedure because of double-inlet left ventricle and
pulmonary atresia. For primary prevention due to severe LV
failure, the ICD lead was placed subcutaneously along the
contour of the left chest wall and the rate-sensing lead was
attached directly to the epicardium through a lateral mini-
thoracotomy. Both were then connected to the ICD generator
placed in the sub-pectoral region. There were no major
cardiovascular complications.
It is not clear from the literature which non-traditional
method is the best in patients with Fontan and other limited
venous access. In a review of multicentre experiences, the authors
have described several ICD implantation techniques that did not
utilise either transvenous high-voltage coils or epicardial patches
in children and young adults.
22
A total of 22 patients (mean age 9 ± 10 years) underwent
a novel ICD implant approach at the 10 centres. Diagnoses
included several types of complex congenital heart disease:
intracardiac tumours (
n
= 2), hypertrophic cardiomyopathy (
n
=
1), long QT syndrome (
n
= 4), left ventricular non-compaction
(
n
= 1), ARVD (
n
= 1) and idiopathic VT or VF (
n
= 6). Three
different configurations for the coil were used; 11 patients had
subcutaneous arrays placed around the thorax, eight had a
transvenous design ICD lead placed on the epicardium, one
had a transvenous design lead placed on the epicardium as
well as subcutaneous arrays added due to a high defibrillation
threshold with the epicardial lead alone, and two patients has a
transvenous design ICD lead placed in a subcutaneous position.
Most patients underwent a thoracotomy or limited subxiphoid
sternotomy for placement of either an epicardial coil and/or
ventricular pace-sense lead. A comparison was made between
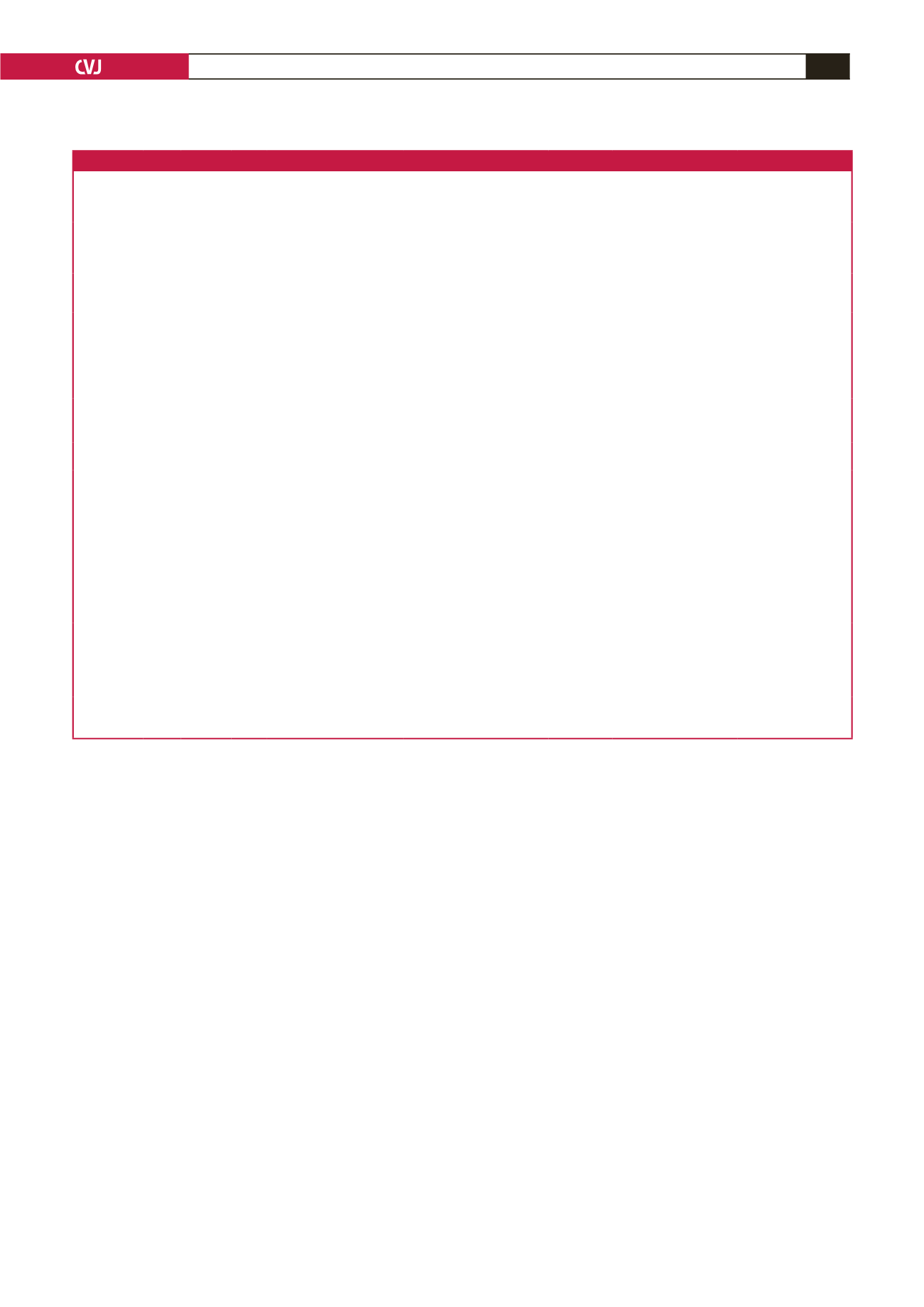
Table 1. Arrhythmias late after the Fontan operation in some studies
Authors
Follow
up
(years)
Patients
(
n
)
Mean
age at
Fontan
(year) Bradyarrhythmia
Supraventricular arrhythmias
Ventricular
arrhythmias Treatment
Outcome
Driscoll
et al
.
(1992)
2
7.7
352
11.1 PM implantation (13%)
AF/AFL (21%)
PVC (11%)
VT (6%)
Anti-arrhythmic drugs
Death (35%)
Reoperation (29%)
Hospitalisation for
arrhythmias (15%)
Gates
et al
.
(1997)
8
7.4
21
27 Complete heart block (5%)
Atrial arrhythmias (37%)
VA (11%) Anti-arrhythmic drugs
Operative mortality (5%)
Late death (5%)
Reoperation (16%)
Durongpisitkul
et al.
(1998)
9
5.9
499
9.5 Sinus bradycardia (3.4%)
Junctional rhythm (6.1%)
SVT (all types)
(17% at 5 years)
PM implantation
Early mortality 9%
5-year mortality: 13%
Sudden death 29%
Late SVT risk factors;
Age at operation (
<
3 or
≥
10 years)
AV valve replacement
Van den Bosch
et al.
(2004)
10
15
36
12 SND (17%)
AV block (6%)
SVT (56%)
VT (6%) Epicardial PM implantation
Anti-arrhythmic drugs
Catheter ablation
Deaths (28%)
Arrhythmogenic deaths
(11%)
Nürnberg
et al.
(2004)
11
7.9
4.4
ILT (29)
ECC (45)
5.8
3.8
Late bradyarrhythmia (11.5%)
(0)
Late SVT (27%)
(0)
PM implantation
Total mortality (8%)
Stephenson
et
al.
(2010)
12
8.6
520
3.4 Bradycardia (5%)
SND (1.3%)
Junctional rhythm (0.3%)
Complete heart block (0.2%)
Ectopic atrial tachycardia (0.8%)
AVRT (1.8%)
IART (7.3%)
VT (3.5%) PM implantation (12%)
ICD implantation (0.9%)
IART increased with
age; mean age for IART
14.4 years
Nakamura
et
al.
(2011)
13
18.5 APC (26)
TCPC (22)
5
AT/IART (58%)
AF (12%)
SVT (41%)
NS-VT (15%)
(9%)
Fontan conversion
Full maze procedure
Anti-arrhythmic drugs
Electrophysiologic study
Catheter ablation
Balaji
et al.
(2013)
14
9.2 ILT (602)
ECC (669)
Late bradyarrhythmia (18%)
(9%)
Late tachyarrhythmia
(10%)
(3%)
–
DC cardioversion (acute)
(7%)
(2%)
Lasa
et al.
(2014)
15
7.1
10.5
ECC (87)
ILT (106)
2.4
1.9
Bradyarrhythmia (30%)
– SND (
n
= 25)
– SND (
n
= 32)
– Complete heart block (
n
= 1)
Tachyarrhythmia (7%)
– AVNRT (
n
=
1)
– IART (
n
=
2)
AVNRT (
n
=
1)
IART (
n
=
3)
JET (
n
=
1)
–
PM implantation
(
n
=
2)
(
n
=
12)
Duration of follow up
from Fontan was an
independent predictor of
late PM implantation
PM: pacemaker, AF: atrial fibrillation, AFL: atrial flutter, PVC: premature ventricular contraction, VT: ventricular tachycardia, VA: ventricular arrhythmias, SVT: supraventricular
tachycardia, AVRT: re-entrant atrio-ventricular tachycardia, IART: intra-atrial re-entrant tachycardia, AT: atrial tachycardia, JET: junctional ectopic tachycardia, SND: sinus node
dysfunction, LTFO: intra-atrial lateral tunnel, ECC: extra-cardiac conduit, APC: atrio-pulmonary connection, TPCP: total cavo-pulmonary connection.



















